| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website https://www.thejh.org |
Case Report
Volume 10, Number 5, October 2021, pages 221-227
Hemolytic Anemia Complicating COVID-19 Infection
Abeer N. AbouYabisa, b, Grace Thompson Bella
aDepartment of Hematology and Oncology, Emory University, Atlanta, GA, USA
bCorresponding Author: Abeer N. AbouYabis, Department of Hematology and Oncology, Emory University School of Medicine, 550 Peachtree St NE, MOT Suite 1075, Rm 1001, Atlanta, GA 30308, USA
Manuscript submitted August 9, 2021, accepted September 17, 2021, published online October 5, 2021
Short title: Hemolytic Anemia Complicating COVID-19 Infection
doi: https://doi.org/10.14740/jh906
| Abstract | ▴Top |
Coronavirus disease 2019 (COVID-19) has been associated with a spectrum of reported hematological complications ranging from immune cytopenias to thromboembolic manifestations of coagulopathy. Moreover, there have been documented cases of hemolytic anemia associated with COVID-19 infection which have been mainly attributed to development of autoantibodies. We report a case of an African-American patient who presented with hemolytic anemia in the second week after his COVID-19 diagnosis. Throughout this report, we explore the potential immune and non-immune etiologies that contributed to the patient’s hemolytic anemia in the setting of COVID-19 infection guided by a review of literature.
Keywords: Hemolytic anemia; COVID-19; Autoimmune hemolytic anemia; G6PD deficiency
| Introduction | ▴Top |
Coronavirus disease 2019 (COVID-19) infection is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) strain and has been associated with a wide spectrum of disease manifestations ranging from asymptomatic disease to a severe inflammatory cytokine storm affecting multiple organ systems. The most commonly reported hematological complications of COVID-19 infection have been cytopenia, coagulopathy and thromboembolic events [1-3].
We report here an African-American patient with hemolytic anemia in the setting of positive direct antiglobulin test (DAT) and within the timeframe of COVID-associated cytokine storm. Given the timeframe and setting, this could be labeled as COVID-19-associated autoimmune hemolytic anemia (AIHA) supported by the growing number of reported cases of AIHA presenting during SARS-CoV-2-induced hyper-inflammatory state (Table 1) [4-20]. However, a negative eluate along with delayed and suboptimal response to steroids triggered a search for another contributory mechanism for hemolysis. Given patient’s ethnic background, a glucose-6-phosphate dehydrogenase (G6PD) level was ordered, and results confirmed deficiency which we think contributed significantly to patient’s hemolysis. This report further investigates the potential mechanisms of hemolysis that can be associated with COVID-19 infection and is the first to raise the possibility of COVID-19 infection as an infectious trigger for hemolysis in patients with G6PD deficiency.
 Click to view | Table 1. Literature Review of Autoimmune Hemolytic Anemia Associated With COVID-19 |
| Case Report | ▴Top |
A 54-year-old African-American man presented to the emergency department reporting a 103 °F temperature and 2-week history of worsening shortness of breath, cough, fatigue and nausea. He had tested negative for SARS-CoV-2 twice during those 2 weeks; however, 9 days prior to presentation, a third SARS-CoV-2 polymerase chain reaction (PCR) resulted positive. A positive SARS-CoV-2 PCR was confirmed upon admission. Three weeks prior to presentation, he had a tooth infection for which he took amoxicillin for 5 days. He had no history of anemia, drug allergies or blood transfusions.
On admission patient was afebrile, in no acute distress, hemodynamically stable with no significant findings on physical exam as summarized in Table 2.
 Click to view | Table 2. Vital Signs and Physical Exam Findings |
A complete blood count (CBC) revealed hemoglobin (Hgb) of 6.7 g/dL, with leukocytosis and normal platelet count. Indirect antiglobulin test (IAT) was positive with no alloantibody identified. Lactate dehydrogenase (LDH) and total bilirubin were elevated while haptoglobin was low (Table 3). DAT on admission was weakly positive for complement C3 and negative immunoglobulin G (IgG). G6PD was later found to be decreased at 3.1 U/g of Hgb. Viral workup was negative except for COVID-19. Creatinine was elevated > 5 mg/dL on admission with workup suggestive of acute tubular necrosis secondary to COVID-19 that improved during hospitalization. Chest X-ray demonstrated bilateral airspace opacities consistent with SARS-CoV-2 infection. Ultrasound of the lower extremities performed due to right leg pain was positive for deep vein thrombosis and patient was started on anticoagulation. Other diagnostic findings are summarized in Table 4.
 Click to view | Table 3. Laboratory Findings |
 Click to view | Table 4. Diagnostic Findings |
Patient received one unit of packed red blood cells (PRBCs) on admission and subsequent daily transfusions with no significant improvement in Hgb. Prednisone 1 mg/kg was also started on admission. On day 3, his DAT became positive for IgG (2+) and complement C3 (3+). Eluate was non-reactive. Patient was switched to dexamethasone 40 mg orally daily for 4 days on day 5 as Hgb continued to be below 7 g/dL with daily transfusions. Hgb trend in response to steroid treatment is depicted in Figure 1. Rituximab was not given in setting of COVID-19 infection. When Hgb dropped again to lower than 7 g/dL after initial improvement on dexamethasone, prednisone 60 mg daily was restarted. Hgb increased to 9.3 g/dL and patient became transfusion-independent. Patient was discharged on day 14 of admission and continued prednisone taper outpatient over 2 weeks with stabilization of Hgb at 8.5 g/dL. DAT became negative 4 weeks after initial diagnosis of AIHA. Patient was re-admitted 3 weeks after discharge with multifocal pneumonia and treated with antibacterial agents. His Hgb remained 8 - 8.5 g/dL during his second hospitalization with negative DAT and no evidence of hemolysis. In the outpatient setting, his Hgb continued to fluctuate between 8.5 and 10.5 g/dL with no obvious underlying cause of persistent anemia. A bone marrow biopsy was done and revealed mildly hypocellular marrow (20-30%) with no dysplasia or abnormal hematolymphoid cell populations.
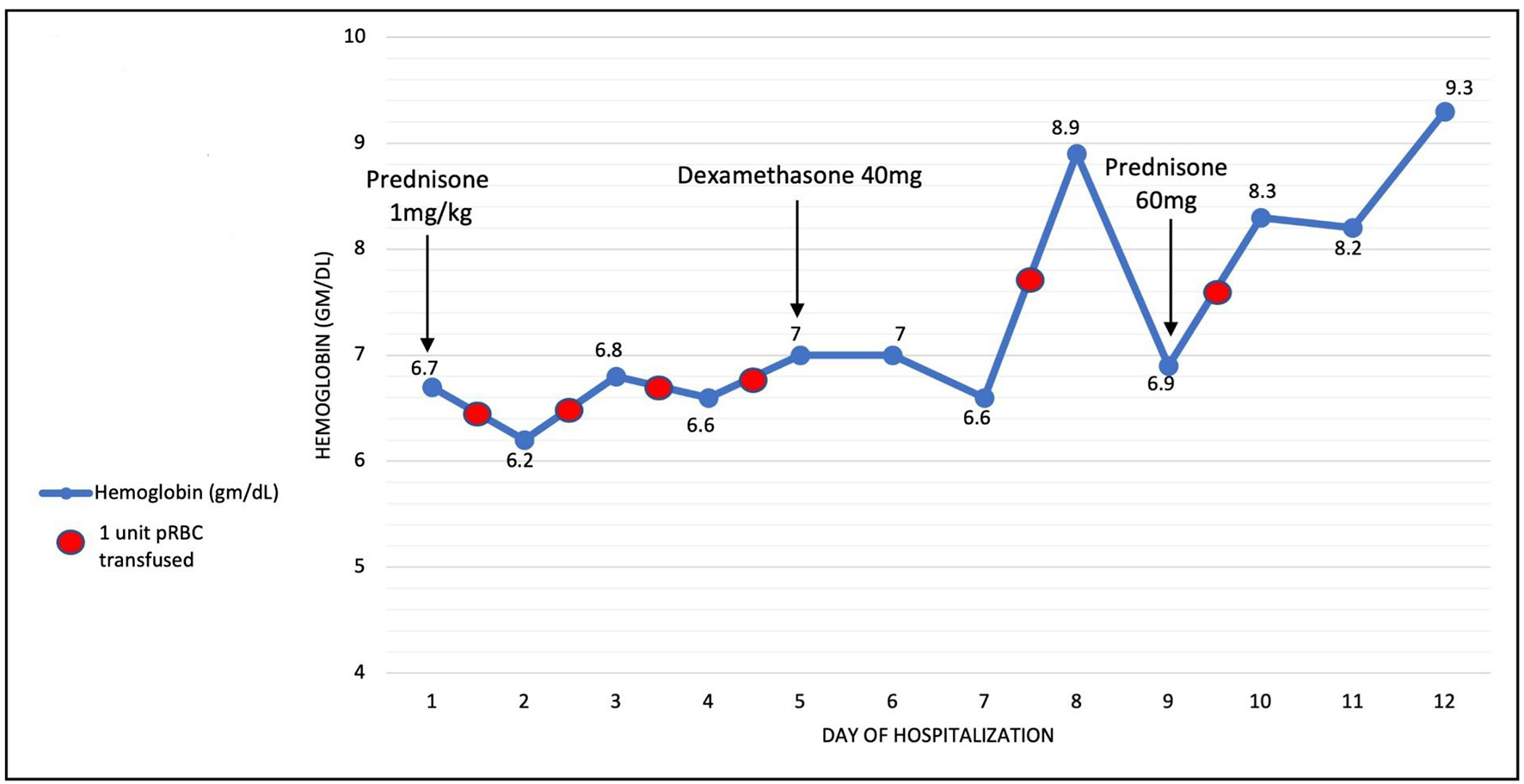 Click for large image | Figure 1. Hemoglobin throughout hospitalization. Arrows indicate start date of medications. Red circles indicate blood transfusion. |
Review of literature
We conducted a computerized literature research to identify publications on AIHA in adult COVID-19 patients using PubMed, Google Scholar and EMBASE from January 1, 2020 to July 31, 2021. The following keywords were used: autoimmune hemolysis, autoimmune hemolytic anemia, COVID-19 and SARS-CoV-2. The references of studies or reports were checked to confirm positive DAT (direct Coombs) as well as positive COVID test upon diagnosis of AIHA.
A total of 26 cases of AIHA associated with COVID-19 infection have been reported to date (Table 1). Both warm and cold autoantibodies have been implicated in COVID-19-associated AIHA.
Time of onset of autoimmune hemolysis was variable; however, most cases were diagnosed in the first 2 weeks of infection. Only one case was reported after 7 weeks of COVID-19 diagnosis [6]. Five reported cases had underlying hematologic malignancy that could have contributed to the development of AIHA [12].
The majority of patients were treated with steroids, only three received rituximab [10, 14] and three received intravenous immunoglobulins [7, 13, 15]. There has not been a consistent definition of remission among different reports and most patients did not have follow-up beyond discharge. However, from available data, it can be concluded that most patients achieved Hgb ≥ 8 g/dL within 14 days of diagnosis (Table 1).
To date, there are no reported cases of G6PD deficiency-associated hemolysis complicating COVID-19 infection.
| Discussion | ▴Top |
We report a case of hemolytic anemia presenting 9 days after positive SARS-CoV-2 PCR test and coinciding with worsening respiratory symptoms and increased inflammatory markers. We propose that the patient’s hemolysis has both immune and non-immune components. Immune-mediated hemolysis is supported by the positive DAT and lack of response to transfusions. Patient’s G6PD deficiency likely played an additional role in the severity of anemia, suboptimal response to steroids and delayed remission.
Drug-induced immune hemolytic anemia was first considered given the weakly positive complement-only DAT and later non-reactive eluate. The possible culprit was the amoxicillin which the patient took within 2 weeks prior to admission. However, this does not explain patient’s worsening symptoms, continued hemolysis requiring transfusion, and increase in the strength of DAT positivity (2+ IgG and 3+C3) 3 days after admission and more than 1 week after stopping amoxicillin.
Since the patient’s immune-mediated hemolysis coincided with worsening COVID-19 symptoms within the timeframe compatible with COVID-associated cytokine storm, SARS-CoV-2-mediated immune hemolysis became high on the differential. There is a growing number of reported cases of AIHA in the setting of COVID infection presenting during SARS-CoV-2-induced hyper-inflammatory state (Table 1). The exact mechanism of AIHA in the setting of COVID-19 infection remains unknown. One proposed mechanism is that the SARS-CoV-2 cytokine-rich inflammatory environment causes alteration in antigen presentation creating cryptic antigens [21]. Those cryptic antigens stimulate T lymphocytes which in turn activates autoreactive B lymphocytes to produce antibodies against those antigens [21-23]. These antibodies then coat the red blood cells (RBCs) causing the positive DAT in around 44-46% of COVID-19 patients [21, 24]. The importance of the COVID-induced inflammatory milieu in exposing cryptic antigens was further emphasized by demonstrating that the DAT can be “transmitted” to allogeneic RBCs that have been in contact with the plasma of DAT-positive COVID-19 patients [21, 23]. In their study, Brochier et al reported a negative eluate among all of the 99 hospitalized COVID-19 patients who had a positive DAT [21], a finding similar to that of our patient. The number of COVID-19 patients with positive DAT who would eventually develop clinically significant hemolysis remains unknown. Since reporting on AIHA in the setting of COVID-19 has been limited to few case reports, it is not clear if other factors would contribute to the development and severity of hemolysis in those COVID-19 patients with positive DAT.
The patient we are reporting here has G6PD deficiency which we believe contributed to his worsening hemolysis and prolonged anemia. Our patient was treated with amoxicillin 2 weeks prior to presentation. Amoxicillin-induced hemolysis in G6PD-deficient patients has been reported [25]. However, a positive DAT and hemolysis that developed more than 7 days after the last dose of amoxicillin make it an unlikely culprit. On the other hand, there have been several pieces of evidence suggesting that G6PD deficiency may increase susceptibility to, and severity of illness associated with COVID-19 infection [26, 27]. RBC destruction in otherwise asymptomatic patients with G6PD deficiency can be triggered by certain infectious agents and medications where decreased production of G6PD results in deficient levels of nicotinamide adenine dinucleotide phosphate and reduced glutathione, causing oxidative stress and RBC destruction. COVID-19 infection could be among those infectious triggers for hemolysis in patients with G6PD deficiency. In light of growing evidence that African-American patients are disproportionately affected by severe COVID-19 infection and given increased prevalence of G6PD deficiency among African-American patients, further studies are needed to determine whether a positive correlation exists between G6PD deficiency and COVID-19 with respect to increased susceptibility to infection and severity of illness [26-28].
Conclusion
Hemolytic anemia in the setting of SARS-CoV-2 appears multifactorial. The exact mechanism of autoimmune hemolysis in COVID-19 infection requires further elucidation. G6PD deficiency is another factor that requires additional consideration especially in patients who belong to ethnic groups where G6PD deficiency is prevalent and demonstrate hemolysis in the setting of acute COVID-19 infection.
Acknowledgments
The authors would like to express sincere gratitude to Dr. Christine Kempton for reviewing the manuscript and to the patient for giving permission to share his case.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Consent was obtained from the patient.
Author Contributions
All authors contributed to the editing of the manuscript. ANA wrote the manuscript. GTB made the accompanying tables and figure. All authors read and approved the final manuscript.
Data Availability
The data that support the findings of this study are available from the electronic medical records of the patient. Data are available from the authors upon reasonable request and with permission of the patient.
| References | ▴Top |
- Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135(23):2033-2040.
doi pubmed - Klok FA, Kruip M, van der Meer NJM, Arbous MS, Gommers D, Kant KM, Kaptein FHJ, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145-147.
doi pubmed - Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061-1069.
doi pubmed - Campos-Cabrera G, Mendez-Garcia E, Mora-Torres M, et al. Autoimmune hemolytic anemia as initial presentation of COVID-19 infection. Blood. 2020;136(Supplement1):8.
doi - Capes A, Bailly S, Hantson P, Gerard L, Laterre PF. COVID-19 infection associated with autoimmune hemolytic anemia. Ann Hematol. 2020;99(7):1679-1680.
doi pubmed - Pelle MC, Tassone B, Ricchio M, Mazzitelli M, Davoli C, Procopio G, Cancelliere A, et al. Late-onset myocardial infarction and autoimmune haemolytic anaemia in a COVID-19 patient without respiratory symptoms, concomitant with a paradoxical increase in inflammatory markers: a case report. J Med Case Rep. 2020;14(1):246.
doi pubmed - Hindilerden F, Yonal-Hindilerden I, Akar E, Yesilbag Z, Kart-Yasar K. Severe autoimmune hemolytic anemia in COVID-19 infection, safely treated with steroids. Mediterr J Hematol Infect Dis. 2020;12(1):e2020053.
doi pubmed - Hsieh TC, Sostin O. Severe warm autoimmune hemolytic anemia in COVID-19 managed with least incompatible RBC product and glucocorticoids. Ann Hematol. 2021.
doi pubmed - Huda Z, Jahangir A, Sahra S, Rafay Khan Niazi M, Anwar S, Glaser A, Jahangir A. A case of COVID-19-associated autoimmune hemolytic anemia with hyperferritinemia in an immunocompetent host. Cureus. 2021;13(6):e16078.
doi - Jacobs J, Eichbaum Q. COVID-19 associated with severe autoimmune hemolytic anemia. Transfusion. 2021;61(2):635-640.
doi pubmed - Jawed M, Hart E, Saeed M. Haemolytic anaemia: a consequence of COVID-19. BMJ Case Rep. 2020;13(12):e238118.
doi pubmed - Lazarian G, Quinquenel A, Bellal M, et al. Autoimmune hemolytic anemia associated with COVID-19 infection. Br J Haematol. 2020;190(1):29-31.
doi pubmed - Li M, Nguyen CB, Yeung Z, Sanchez K, Rosen D, Bushan S. Evans syndrome in a patient with COVID-19. Br J Haematol. 2020;190(2):e59-e61.
doi - Liput JR, Jordan K, Patadia R, Kander E. Warm autoimmune hemolytic anemia associated with asymptomatic SARS-CoV-2 infection. Cureus. 2021;13(3):e14101.
doi pubmed - Lopez C, Kim J, Pandey A, Huang T, DeLoughery TG. Simultaneous onset of COVID-19 and autoimmune haemolytic anaemia. Br J Haematol. 2020;190(1):31-32.
doi pubmed - Patil NR, Herc ES, Girgis M. Cold agglutinin disease and autoimmune hemolytic anemia with pulmonary embolism as a presentation of COVID-19 infection. Hematol Oncol Stem Cell Ther. 2020.
doi - Raghuwanshi B. Serological blood group discrepancy and cold agglutinin autoimmune hemolytic anemia associated with novel coronavirus. Cureus. 2020;12(11):e11495.
doi - Ramos-Ruperto L, Garcia-Perez E, Hernandez-Maraver D, Kerguelen-Fuentes A, Viejo-Llorente A, Robles-Marhuenda A, Busca-Arenzana C. A 3-case series of autoimmune haemolytic anaemia and COVID-19: is plasma exchange an alternative? SN Compr Clin Med. 2021;3:1420-1423.
doi pubmed - Woldie IL, Brown IG, Nwadiaro NF, Patel A, Jarrar M, Quint E, Khokhotva V, et al. Autoimmune hemolytic anemia in a 24-year-old patient with COVID-19 complicated by secondary cryptococcemia and acute necrotizing encephalitis: a case report and review of literature. J Med Cases. 2020;11(11):362-365.
doi pubmed - Zagorski E, Pawar T, Rahimian S, Forman D. Cold agglutinin autoimmune haemolytic anaemia associated with novel coronavirus (COVID-19). Br J Haematol. 2020;190(4):e183-e184.
doi pubmed - Brochier A, Cabo J, Guerrieri C, et al. Autoimmune hemolytic anemia in COVID-19 patients, the "transmissible" direct Coombs test. J Hematol and Clin Research. 2021;5:004-008.
doi - Fagiolo E, Toriani-Terenzi C. Mechanisms of immunological tolerance loss versus erythrocyte self-antigens and autoimmune hemolytic anemia. Autoimmunity. 2003;36(4):199-204.
doi pubmed - Prasad S, Starck SR, Shastri N. Presentation of cryptic peptides by MHC class I is enhanced by inflammatory stimuli. J Immunol. 2016;197(8):2981-2991.
doi pubmed - Berzuini A, Bianco C, Paccapelo C, Bertolini F, Gregato G, Cattaneo A, Erba E, et al. Red cell-bound antibodies and transfusion requirements in hospitalized patients with COVID-19. Blood. 2020;136(6):766-768.
doi pubmed - Blanquicett CJ, Raavi T, Robert SM. A severe episode of hemolytic anemia after amoxicillin exposure in a G6PD deficient patient. Arch Clin Med Case Rep. 2019;3(3):104-112.
doi pubmed - Vick DJ. Glucose-6-phosphate dehydrogenase deficiency and COVID-19 infection. Mayo Clin Proc. 2020;95(8):1803-1804.
doi pubmed - Wu YH, Tseng CP, Cheng ML, Ho HY, Shih SR, Chiu DT. Glucose-6-phosphate dehydrogenase deficiency enhances human coronavirus 229E infection. J Infect Dis. 2008;197(6):812-816.
doi pubmed - Gold JAW, Wong KK, Szablewski CM, Patel PR, Rossow J, da Silva J, Natarajan P, et al. Characteristics and clinical outcomes of adult patients hospitalized with COVID-19 - Georgia, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69(18):545-550.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


