| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website https://www.thejh.org |
Case Report
Volume 10, Number 5, October 2021, pages 217-220
Acute Respiratory Distress Syndrome in a Patient With Acute Promyelocytic Leukemia: Overlapping Between Differentiation Syndrome and COVID-19
Jingrui Suia, b, Daniel Kelmensonc, Shimin Hud, Liyun Caoa, e
aDivision of Laboratory Medicine, Department of Pathology, The University of Alabama at Birmingham, Birmingham, AL, USA
bDepartment of Hematology, The Affiliated Yantai Yuhuangding Hospital of Qingdao University, Yantai, China
cDivision of Pulmonary, Allergy & Critical Care Medicine, Department of Medicine, The University of Alabama at Birmingham, Birmingham, AL, USA
dDepartment of Hematopathology, The University of Texas MD Anderson Cancer Center, Houston, TX, USA
eCorresponding Author: Liyun Cao, Division of Laboratory Medicine, Department of Pathology, The University of Alabama at Birmingham, Birmingham, AL 35249, USA;
Manuscript submitted July 30, 2021, accepted September 2, 2021, published online September 15, 2021
Short title: Overlapping of DS and COVID-19
doi: https://doi.org/10.14740/jh904
| Abstract | ▴Top |
Differentiation syndrome (DS) is a relatively common and severe complication in acute promyelocytic leukemia (APL) patients undergoing induction therapy with all-trans retinoic acid (ATRA) and/or arsenic trioxide (ATO). DS is a multisystem disorder with pulmonary involvement. The coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection is also a systemic disorder with similar pulmonary and other clinical manifestations as DS. Here, we report an APL case with overlapping between DS and COVID-19. After admission to the hospital, the patient was diagnosed with APL and underwent differentiation therapy with ATRA/ATO. In the meantime, COVID-19 was diagnosed with a positive polymerase chain reaction test of SARS-CoV-2 from an oropharyngeal swab. The patient developed acute respiratory distress syndrome, coagulopathy, and acute kidney injury, which fit the clinical pictures of both DS and COVID-19. The patient died at last and this complicate case imposed big challenges for clinicians due to the laboratory and imaging findings of DS disguised in the context of COVID-19. Therefore, comprehensive treatment strategy should be considered to balance the risk and benefit of differentiation therapy in the context of COVID-19.
Keywords: Acute promyelocytic leukemia; Differentiation syndrome; Coronavirus disease 2019; Acute respiratory distress syndrome
| Introduction | ▴Top |
Acute promyelocytic leukemia (APL) is characterized with translocation between chromosomes 15 and 17 (t(15;17)). This translocation results in the formation of an abnormal fusion gene PML/RARα, which is the target of the all-trans retinoic acid (ATRA). Differentiation syndrome (DS) is a relatively common and severe complication in APL patients after treatment with ATRA and/or arsenic trioxide (ATO). DS is a multisystem disorder with pulmonary involvement. On the other hand, the coronavirus disease 2019 (COVID-19) outbreak poses extra challenges to the management of patients with leukemia. Due to the immunosuppression from the underlying cancer and from the correspondent therapy, leukemia patients are at increased risk of viral infection and adverse outcomes. COVID-19 may mimic DS by its similar clinical presentations, which can cause a challenge for disease diagnosis and patient management. Here we report an APL patient who developed acute respiratory distress syndrome (ARDS) after ATRA/ATO treatment during the COVID-19 pandemic.
| Case Report | ▴Top |
A 62-year-old man with a history of type 2 diabetes, hypertension, hyperlipidemia, and obesity was admitted to an outside hospital due to progressive fatigue, weakness, dyspnea, and easy bleeding. He was diagnosed APL with t(15;17)/PML-RARA confirmed by fluorescence in situ hybridization analysis.
The patient was then transferred to our institution. At admission, the patient had a temperature of 38.6 °C, respiratory rate of 18 breaths/min, and SpO2 94% on room air. Laboratory analysis revealed pancytopenia with a white blood cell count of 3.1 × 109 cells/L, neutrophil of 0.34 × 109 cells/L, red blood cell of 1.94 × 109 cells/L, hemoglobin of 6.8 g/dL, and platelet of 4.4 × 109 cells/L. Differential count revealed 38% blasts. Flow cytometric analysis of peripheral blood showed a population of aberrant myeloblasts comprising 69% of the total cells that were CD2+/low, CD13+, CD33+, CD34-/heterogeneous, CD38+/low, CD64+, CD117+/low, CD123+, MPO+, cytoplasmic CD3-, CD7-, CD14-, CD15-, CD56-, cytoplasmic CD79a-, HLA-DR-, and TdT-. The diagnosis of APL was confirmed by the detection of PML/RARα by molecular analysis. The normalized copy number of PML/RARα transcript was 554.638. The patient also had coagulopathy with a prothrombin time (PT) of 16.6 s, activated partial thromboplastin time (aPTT) of 36 s, fibrinogen of 142 mg/dL, fibrinogen of 142 mg/dL, and D-dimer of > 20,000 ng/mL. Since the patient complained of headache for the past several days, head computed tomography (CT) was performed and revealed a very small volume of subarachnoid hemorrhage in the left medial frontal sulci. Posterioranterior and lateral chest X-ray showed slight left basilar atelectasis and was otherwise unremarkable. In the meantime, COVID-19 was diagnosed with a positive polymerase chain reaction (PCR) test of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from an oropharyngeal swab.
The patient’s neutropenic fever prompted initiation of broad-spectrum antibiotics upon admission. ATRA (tretinoin) at 45 mg/m2 was started on day 1 of admission and ATO at 0.15 mg/kg daily on day 2. Dexamethasone 10 mg daily was initiated on day 3 for prophylaxis of DS, which is a relatively common and life-threatening complication in APL patients undergoing differentiation therapy with ATRA and/or ATO. On day 6, the patient developed ARDS with tachypnea (respiratory rate 40 breaths/min), tachycardia (heart rate 125 beats/min), hypotension (blood pressure 74/64 mm Hg), and hypoxemia (SpO2 60% on room air). A chest CT showed trace bilateral pleural effusions and scattered ground-glass opacities with superimposed consolidations throughout both lungs (Fig. 1). The patient was put on mechanical ventilation. He also developed acute renal failure with creatinine of 1.6 mg/dL. Repeated PCR tests for SARS-CoV-2 on day 9 and day 10 were both positive.
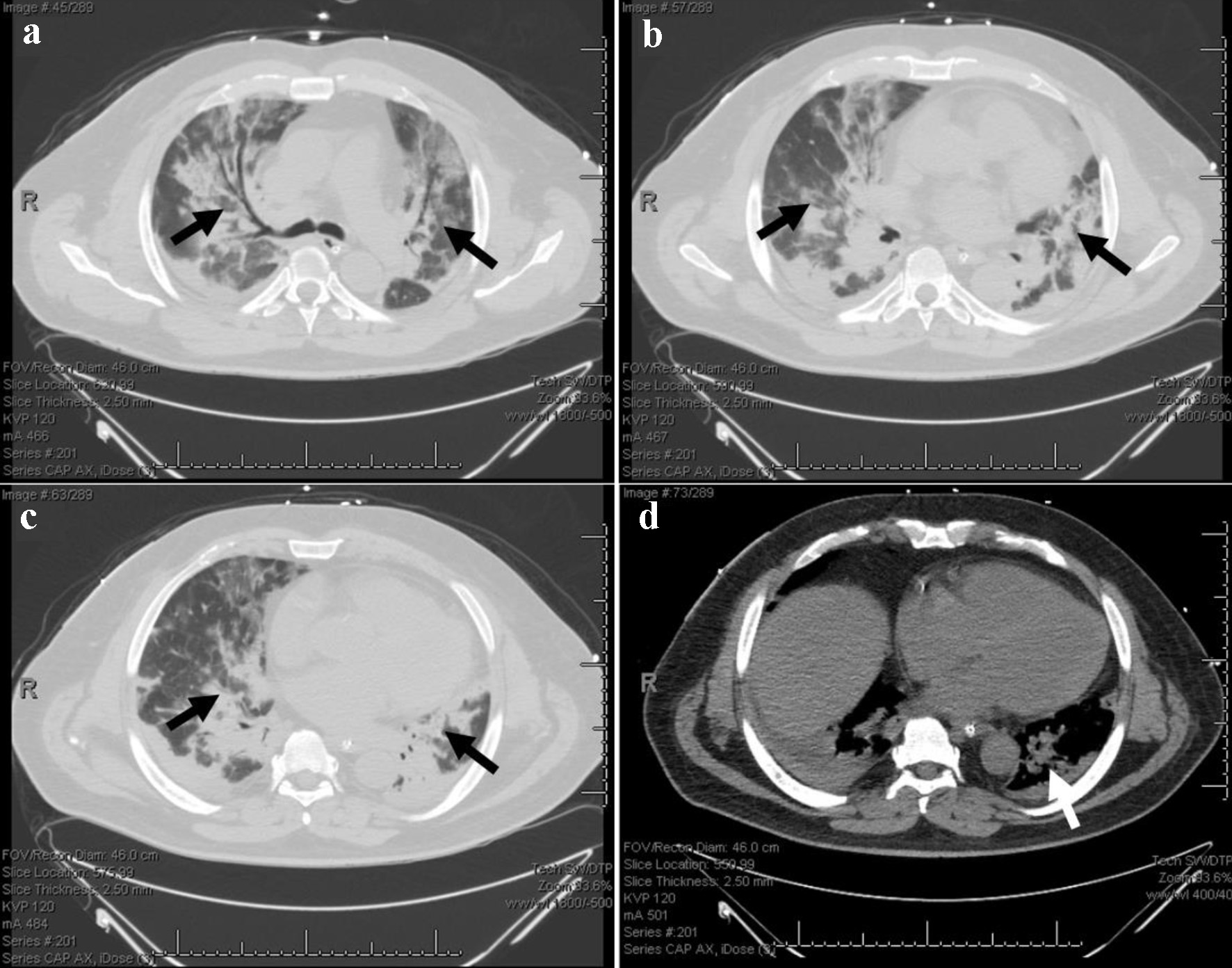 Click for large image | Figure 1. Chest CT on day 6 after admission. (a-c) Bilateral ground-glass opacities and superimposed consolidations. (d) Trace bilateral pleural effusions, right greater than left. The arrows indicate the lesions. CT: computed tomography. |
During hospitalization, the patient’s complete blood count, kidney function, coagulation (Fig. 2), and chest images were continuously monitored and no improvement was observed. His situation was further complicated by transfusion-dependent pancytopenia, hyperglycemia, non-ST segment elevation myocardial infarction, transaminitis, leukemic Sweet syndrome, acute kidney injury, and disseminated intravascular coagulation. Meanwhile, respiratory failure continued to worsen, and acidosis worsened further after continuous renal replacement therapy was discontinued due to multiple line clots. The patient died on day 17. The patient management during the hospitalization was summarized in corresponding with the continuous laboratory monitoring of complete blood count, creatinine, and coagulation (Fig. 3).
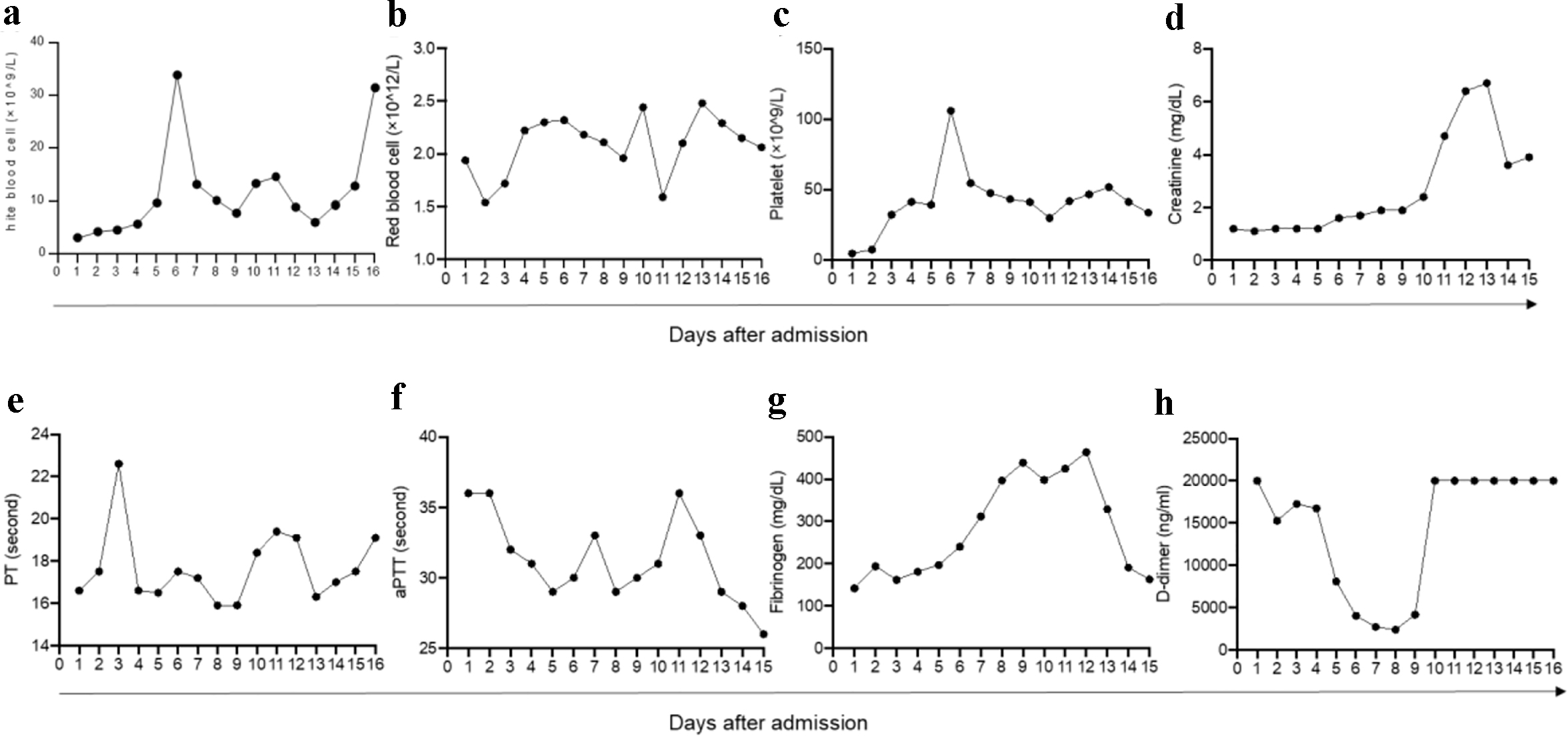 Click for large image | Figure 2. Continuous monitoring of complete blood count, creatinine, and coagulation during hospitalization. (a) White blood cell count (reference range, 4.0 - 11.0 × 109/L). (b) Red blood cell count (reference range, 4.40 - 5.80 × 1012/L). (c) Platelet count (reference range, 150.0 - 400.0 × 109/L). (d) Creatinine (reference range, 0.7 - 1.3 mg/dL). (e-h) Coagulation testing, including PT (reference range, 12.0 - 14.5 s), aPTT (reference range, 25.0 - 35.0 s), fibrinogen (reference range, 220.0 - 498.0 mg/dL), and D-dimer (reference range, 0.0 - 240.0 ng/mL). PT: prothrombin time; aPTT: activated partial thromboplastin time. |
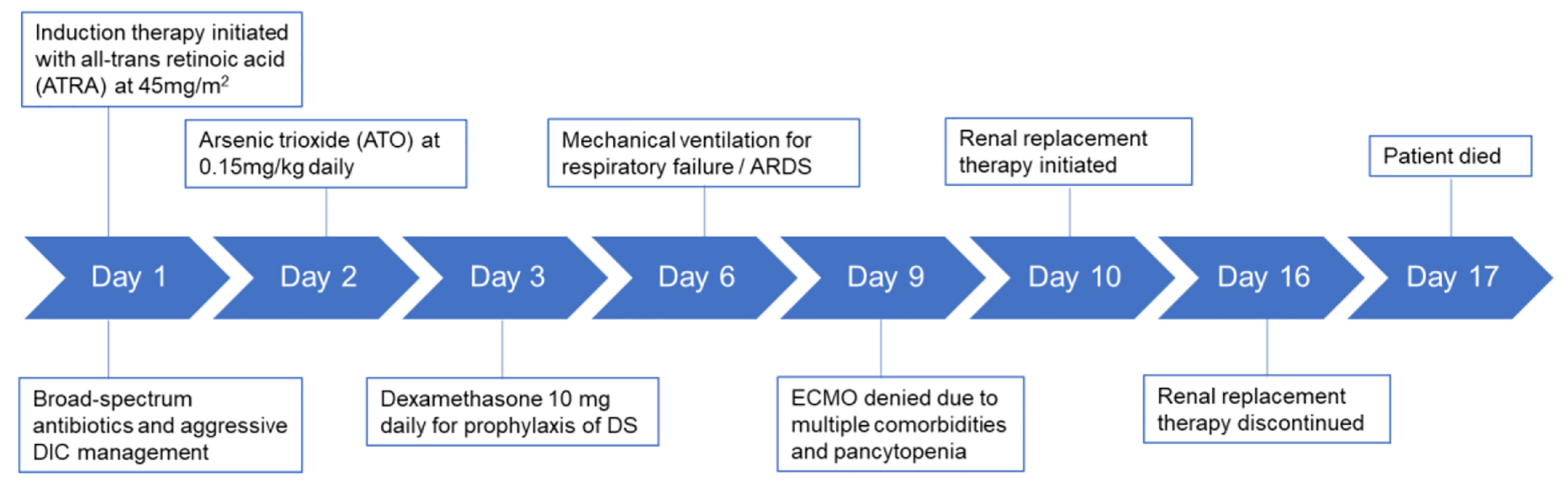 Click for large image | Figure 3. A brief summary of patient management during hospitalization. DIC: disseminated intravascular coagulation; DS: differentiation syndrome; ECMO: extracorporeal membrane oxygenation. |
| Discussion | ▴Top |
DS is a life-threatening complication in patients with APL, characterized by fever, weight gain, hypotension, ARDS, acute renal failure, pulmonary infiltrate, and pleural or pericardial effusion. Currently, there are no definitive diagnostic criteria for DS. The diagnosis of DS is mainly based on the clinical presentation in an appropriate clinical context [1, 2]. This patient had ARDS, fever, hypotension, edema and acute renal failure, and a diagnosis of DS was rendered. Other manifestations associated with DS, such as acute febrile neutrophilic and leukemic Sweet syndrome, were also observed in the patient. However, the patient had a fever at admission and before APL therapy was started, and thus the fever could also be attributable to SARS-CoV-2 infection. Although DS was most likely the cause of ARDS in this patient, COVID-19 related ARDS could not be ruled out due to the persistent SARS-CoV-2 positivity. Furthermore, some clinical and laboratory findings in this patient, such as fever, thrombocytopenia, coagulopathy, and acute renal failure, are also typical features observed in patients with COVID-19 [3]. It is likely that both DS and COVID-19 contributed to the patient’s clinical manifestations. In the era of the COVID-19 pandemic, tests for SARS-CoV-2 infection should be conducted to rule out the coexistence of the disease so that a comprehensive treatment strategy can be adopted to improve the outcome. Recently, the RECOVERY clinical trial reported that dexamethasone at a dose of 6 mg once daily could reduce the 28-day mortality in hospitalized COVID-19 patients [4]. Dexamethasone is also the mainstay of treatment of DS [5]. Therefore, clinicians may consider a dexamethasone regimen that would be beneficial for patients suffering both DS and COVID-19.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained from patient’s daughter.
Author Contributions
JS and LC were involved in the data collection and manuscript preparation. DK was the health-care provider of the patient and involved in revision of the manuscript. SH was involved in preparation and revision of the manuscript.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Stahl M, Tallman MS. Differentiation syndrome in acute promyelocytic leukaemia. Br J Haematol. 2019;187(2):157-162.
doi pubmed - Montesinos P, Sanz MA. The differentiation syndrome in patients with acute promyelocytic leukemia: experience of the pethema group and review of the literature. Mediterr J Hematol Infect Dis. 2011;3(1):e2011059.
doi pubmed - Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054-1062.
doi - Recovery Collaborative Group, Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, et al. Dexamethasone in Hospitalized Patients with Covid-19. N Engl J Med. 2021;384(8):693-704.
doi pubmed - Sanz MA, Montesinos P. How we prevent and treat differentiation syndrome in patients with acute promyelocytic leukemia. Blood. 2014;123(18):2777-2782.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


