| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Case Report
Volume 9, Number 1-2, April 2020, pages 37-40
Diagnostic Dilemma: An Unusual Case of Angioimmunoblastic T-Cell Lymphoma Manifesting as Bone Marrow Non-Caseating Granuloma
Vineel Bhatlapenumarthia, c, Anannya Patwaria, Sheila Karina Pascualb
aNorthern Light Eastern Maine Medical Center, 489 State Street, Bangor, ME 04401, USA
bNorthern Light Cancer Care, 33 Whiting Hill Road, Brewer, ME 04412, USA
cCorresponding Author: Vineel Bhatlapenumarthi, Northern Light Eastern Maine Medical Center, 489 State Street, Bangor, ME 04401, USA
Manuscript submitted February 5, 2020, accepted April 13, 2020
Short title: AITL Manifesting as Non-Caseating Granuloma
doi: https://doi.org/10.14740/jh607
| Abstract | ▴Top |
We present here a rare and unusual presentation of angioimmunoblastic T-cell lymphoma with non-necrotizing granuloma of bone marrow. We did not find any case reports of such case in our literature search. A 77-year-old man presented with shortness of breath, generalized weakness, fatigue and weight loss. Laboratory data revealed elevated white count, low platelets and anemia. Imaging studies revealed generalized lymphadenopathy. A bone marrow biopsy showed hypercellular marrow with non-caseating granuloma which was non-diagnostic and lymph node biopsy showed angioimmunoblastic T-cell lymphoma.
Keywords: Angioimmunoblastic T-cell lymphoma; Lymph node biopsy; CHOP regimen
| Introduction | ▴Top |
Angioimmunoblastic T-cell lymphoma (AITL) is a subtype of peripheral T-cell lymphoma (PTCL), and thought to arise from follicular helper T cell [1]. AITL accounts for approximately 1-2% of non-Hodgkin’s lymphomas and 15-20% of PTCLs. AITL usually affects older adults with a median age of 65 years. Most patients have advanced stage disease at presentation [2]. It is more common in males than in females. Asians are slightly more affected compared to Caucasians and African Americans [3].
Diagnosis is by histological exam of lymph node biopsy. Bone marrow biopsy is usually done to determine the clinical stage of the lymphoma, and bone marrow is usually involved in 60-80% of patients [4].
| Case Report | ▴Top |
A 77-year-old man with past medical history significant for atrial fibrillation, insomnia and post-traumatic stress disorder (PTSD) who has been in his usual state of health presented initially with complaints of shortness of breath on exertion, cough, generalized weakness, fatigue and decreased appetite for almost 2 to 3 weeks. He was initially treated for suspected community-acquired pneumonia with antibiotics. He had a complete blood count (CBC) done that showed white blood cell (WBC) count of 21,000, platelet count of 27,000 and hemoglobin of 12 g/dL. At baseline, he had normal hemoglobin, WBC count and platelet count. Given the abnormal blood test results and lack of any symptomatic improvement, a computed tomography (CT) scan of the chest, abdomen and pelvis was done which showed diffuse lymphadenopathy in the mediastinum (Fig. 1a), axilla (Fig. 1b), retroperitoneal lymphadenopathy (Fig. 1c) and bilateral pleural effusions (Fig. 1d).
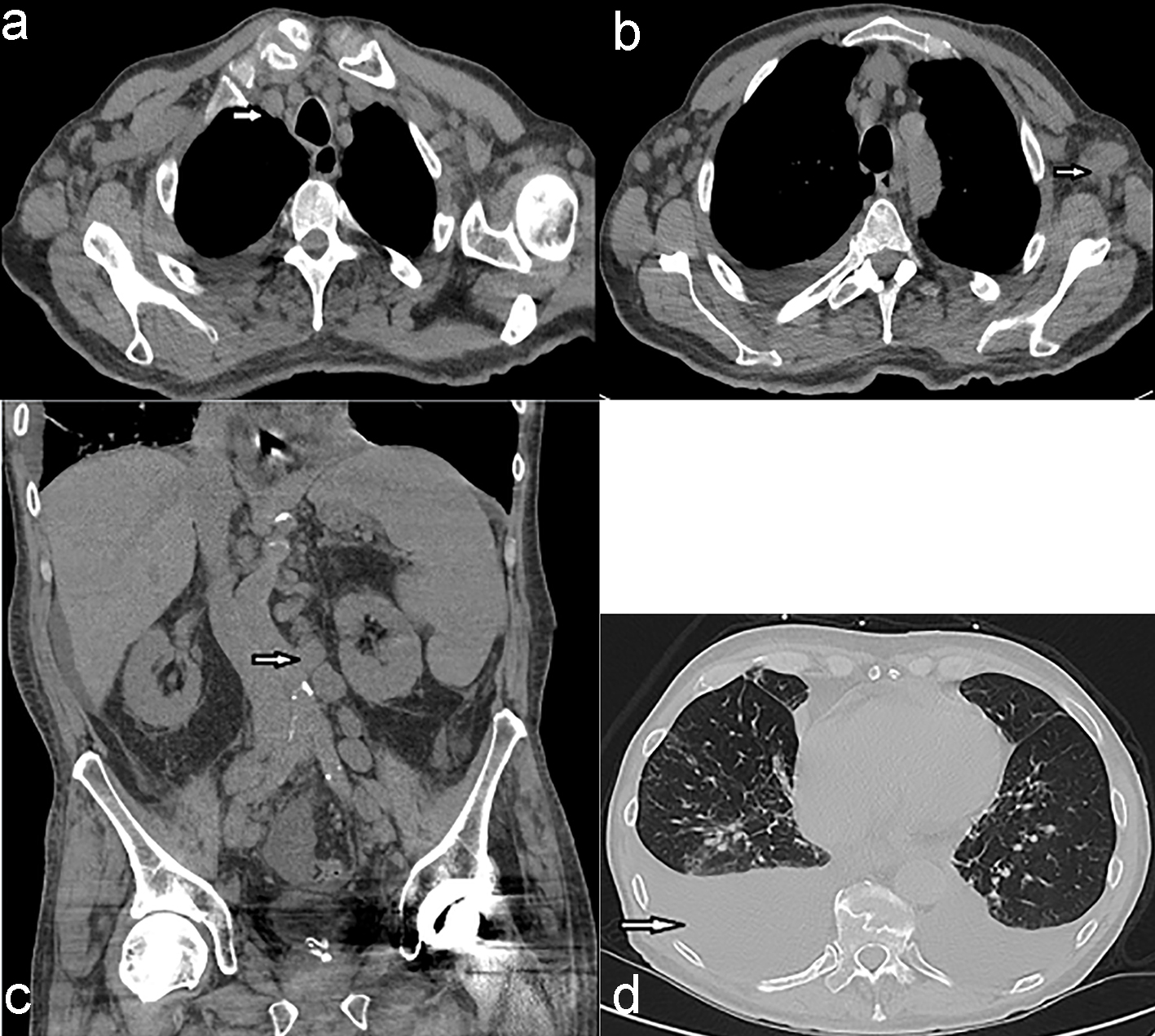 Click for large image | Figure 1. (a) CT scan of the chest showing mediastinal lymphadenopathy (arrow). (b) CT scan of the chest showing axillary lymphadenopathy (arrow). (c) CT of abdomen and pelvis showing retroperitoneal lymphadenopathy (arrow). (d) CT of chest showing bilateral pleural effusions, right more than left (arrow). CT: computed tomography. |
Given the findings of elevated WBC count, thrombocytopenia and diffuse lymphadenopathy, hematology/oncology was consulted. Subsequently, he had a bone marrow biopsy done which showed hypercellular marrow with non-necrotizing granulomatous inflammation (Fig. 2a, b). In view of the diffuse lymphadenopathy and non-necrotizing granulomatous inflammation in bone marrow, a diagnosis of sarcoidosis was considered initially and he was treated with steroids, which did not show any improvement.
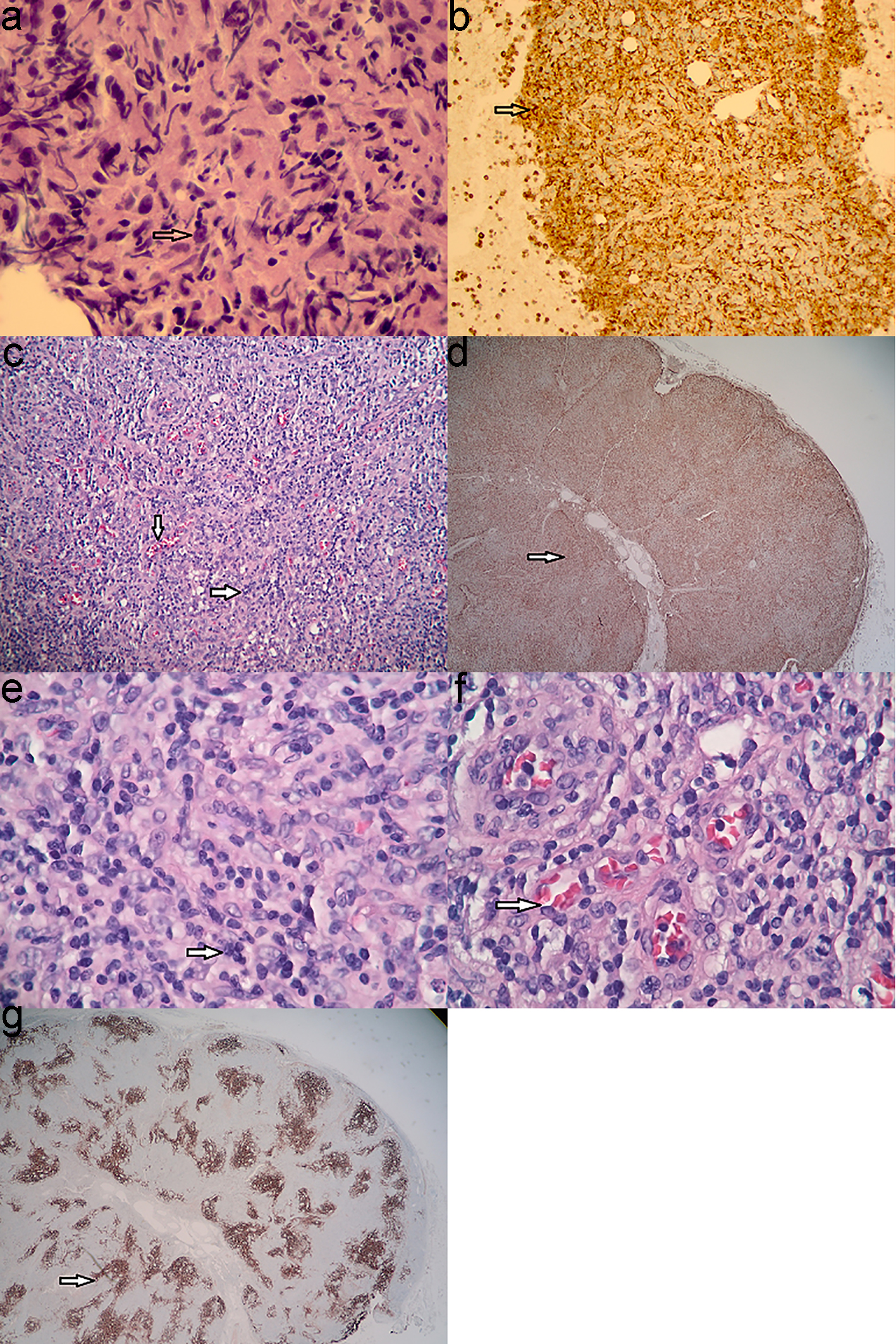 Click for large image | Figure 2. (a) High power view of bone marrow showing non-caseating granuloma with increased histiocytes (arrow). (b) CD68 stain showing increased numbers of histiocytes in bone marrow (arrow). (c) View (× 10) of the lymph node shows increased vasculature in the lymph node (arrow). (d) CD68 stain showing increased numbers of histiocytes in the lymph node (arrow). (e) High power view of the lymph node showing predominantly histiocytes and background small lymphocytes (arrow). (f) High power view of the lymph node showing abundant vessels (arrow). (g) CD21 stain showing follicular dendritic cells (arrow). |
Due to the non-diagnostic bone marrow biopsy and lack of response to steroids, he later underwent a biopsy of the left anterior cervical lymph node. Pathology showed findings consistent with AITL. The sections showed lymph node tissue with architectural effacement by a polymorphous infiltrate predominantly composed of small lymphoid cells with irregular nuclei, inconspicuous nucleoli, coarse chromatin and pale cytoplasm. Scattered larger cells with irregular nuclei, variably prominent nucleoli and moderate pale cytoplasm are also present (Fig. 2c-e). There is an associated arborizing proliferation of vessels (Fig. 2f), follicular dendritic cells (Fig. 2g) and macrophages consistent with AITL. Acid fast bacteria (AFB) and Gomori methenamine silver (GMS) special stains were performed and were negative for mycobacterial and fungal organisms, respectively. In-situ hybridization study for Epstein-Barr virus (EBV)-encoded RNA (EBER) was negative. Proliferation index by Ki-67 was elevated at 30-40%.
Subsequently, the patient was started on chemotherapy with cyclophosphamide, adriamycin, vincristine, prednisone (CHOP) regimen. He received one cycle of the CHOP regimen after which unfortunately he had bowel perforation, and the cause of his bowel perforation was unclear. Later, the patient and family did not want to have any aggressive intervention and chose to keep him comfortable and he subsequently passed away.
| Discussion | ▴Top |
Finding of a granuloma in a bone marrow is not very common. The differential diagnosis for non-caseating granulomas is broad which includes infections like mycobacterial, fungal viral like EBV and cytomegalovirus (CMV), sarcoidosis, autoimmune disorders, toxins, drug induced and other causes like hypersensitivity pneumonitis and lymphomas [5].
One of the most common causes of non-caseating granuloma apart from infectious causes is sarcoidosis. It is mostly associated with pulmonary manifestations. Extrapulmonary manifestations including bone marrow involvement are not uncommon [6]. In our patient initially sarcoid was thought as the diagnosis and he was treated with steroids after the infectious etiologies were ruled out. He did not have any significant response to the steroids that prompted for the lymph node biopsy, which subsequently showed the AITL.
AITL is a rare T-cell lymphoma, and patients usually present at a late stage. B-symptoms such as fevers, unintentional weight loss, and/or drenching night sweats and lymphadenopathy remain the most common presenting complaints. Common physical exam findings include lymphadenopathy, hepatosplenomegaly, skin rash, and ascites/effusions. Most of the patients have generalized lymphadenopathy on presentation as evidenced on CT scan in our patient. The bone marrow findings usually include a polymorphous cell population including small lymphocytes, histiocytes, immunoblasts, eosinophils and plasma cells. The histiocytic component of the infiltrate varies giving a vague granulomatous appearance [7].
The overall prognosis of AITL remains poor with 5-year overall survival at 32% [8]. The treatment modalities for AITL include chemotherapy and autologous stem cell transplant (SCT). There is no gold standard chemotherapy for newly diagnosed AITL, and CHOP chemotherapy is the most commonly used one. The response to chemotherapy is very short lived due to disease progression [9]. Our patient has received CHOP chemotherapy as the upfront regimen. Unfortunately, after one cycle of chemotherapy, he had intestinal perforation and subsequently chose to not to have any aggressive treatments.
Conclusion
AITL is a relatively rare T-cell lymphoma with a poor prognosis. Here we present a patient with AITL whose bone marrow biopsy showed non-caseating granuloma. The presence of bone marrow non-caseating granuloma is not always infection or sarcoidosis. Clinicians should suspect AITL especially in patients where infectious causes have been ruled out and not responding to therapy as in our case. This can lead to early diagnosis and treatment which results in overall improvement in morbidity and mortality. Further research needs to be done on this aspect.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
The manuscript has been sufficiently de-identified to protect the patient. He has since died and is unable to provide informed consent.
Author Contributions
Authors Patwari and Pascual contributed to the editing of the manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Grogg KL, Attygalle AD, Macon WR, Remstein ED, Kurtin PJ, Dogan A. Angioimmunoblastic T-cell lymphoma: a neoplasm of germinal-center T-helper cells? Blood. 2005;106(4):1501-1502.
doi pubmed - Federico M, Rudiger T, Bellei M, Nathwani BN, Luminari S, Coiffier B, Harris NL, et al. Clinicopathologic characteristics of angioimmunoblastic T-cell lymphoma: analysis of the international peripheral T-cell lymphoma project. J Clin Oncol. 2013;31(2):240-246.
doi pubmed - Morton LM, Wang SS, Devesa SS, Hartge P, Weisenburger DD, Linet MS. Lymphoma incidence patterns by WHO subtype in the United States, 1992-2001. Blood. 2006;107(1):265-276.
doi pubmed - Cho YU, Chi HS, Park CJ, Jang S, Seo EJ, Huh J. Distinct features of angioimmunoblastic T-cell lymphoma with bone marrow involvement. Am J Clin Pathol. 2009;131(5):640-646.
doi pubmed - Shah KK, Pritt BS, Alexander MP. Histopathologic review of granulomatous inflammation. J Clin Tuberc Other Mycobact Dis. 2017;7:1-12.
doi pubmed - Eid A, Carion W, Nystrom JS. Differential diagnoses of bone marrow granuloma. West J Med. 1996;164(6):510-515.
- Grogg KL, Morice WG, Macon WR. Spectrum of bone marrow findings in patients with angioimmunoblastic T-cell lymphoma. Br J Haematol. 2007;137(5):416-422.
doi pubmed - Vose J, Armitage J, Weisenburger D, International TCLP. International peripheral T-cell and natural killer/T-cell lymphoma study: pathology findings and clinical outcomes. J Clin Oncol. 2008;26(25):4124-4130.
doi pubmed - Lunning MA, Vose JM. Angioimmunoblastic T-cell lymphoma: the many-faced lymphoma. Blood. 2017;129(9):1095-1102.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


