| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Case Report
Volume 8, Number 3, September 2019, pages 125-128
Incidental Finding of Right Atrial Mass in a Patient With Hodgkin Lymphoma: Utilization of Multimodal Cardiac Imaging in Diagnosis
Abigail Chana, c, Amit Routa, Amteshwar Singha, Sunal Makadiab
aDepartment of Internal Medicine, Sinai Hospital of Baltimore, Baltimore, MD, USA
bInova Heart and Vascular Institute, Fairfax, Virginia, USA
cCorresponding Author: Abigail Chan, Department of Internal Medicine, Sinai Hospital of Baltimore, 2401 W Belvedere Avenue, Baltimore, MD 21215, USA
Manuscript submitted May 14, 2019, accepted July 9, 2019
Short title: Utilization of Imaging in Right Atrial Mass
doi: https://doi.org/10.14740/jh521
| Abstract | ▴Top |
Right atrial masses can be found incidentally on imaging studies, which could represent cardiac or non-cardiac tumors, vegetations, or thrombi. Catheter-related right atrial thrombosis is an uncommon and underdiagnosed condition, but has been associated with significant mortality risk. Herein, we present a case of a 56-year-old man with Hodgkin lymphoma who was found to have a right atrial mass on routine transthoracic echocardiogram. The diagnosis of right atrial thrombus was made by using transesophageal echocardiogram and cardiac magnetic resonance imaging. He was managed with intravenous heparin and was being evaluated for possible thrombectomy when he died from complications of septic shock.
Keywords: Right atrial mass; Catheter-related right atrial thrombus; Cardiac imaging; Hodgkin lymphoma
| Introduction | ▴Top |
Right atrial (RA) masses can be found incidentally on routine imaging studies. RA masses are rare and their management depends on appropriate diagnosis. Catheter-related right atrial thrombosis (CRAT) is uncommon, but its presence carries significant mortality of up to 40% in non-hemodialysis patients [1]. We present a case of RA mass in a patient with Hodgkin lymphoma (HL), in which diagnosis was confirmed with the aid of multimodal cardiac imaging.
| Case Report | ▴Top |
A 56-year-old man was diagnosed with nodular sclerosing cluster of differentiation (CD) 30+, CD15+ HL almost a year prior. He was found to have stage IV disease with diffuse involvement of the lymph nodes, bone marrow and liver. A power-injectable port was inserted and six cycles of ABVD chemotherapy (adriamycin, bleomycin, vinblastine, dacarbazine) was initiated achieving only partial response. He underwent two other lines of chemotherapy, with poor clinical response. He was being evaluated for autologous hematopoietic stem cell transplant (HSCT) when the pretransplant transthoracic echocardiogram (TTE) revealed a 2.2 × 1.8 cm RA mass with normal cardiac function (Fig. 1). He was then sent to the emergency room for further evaluation.
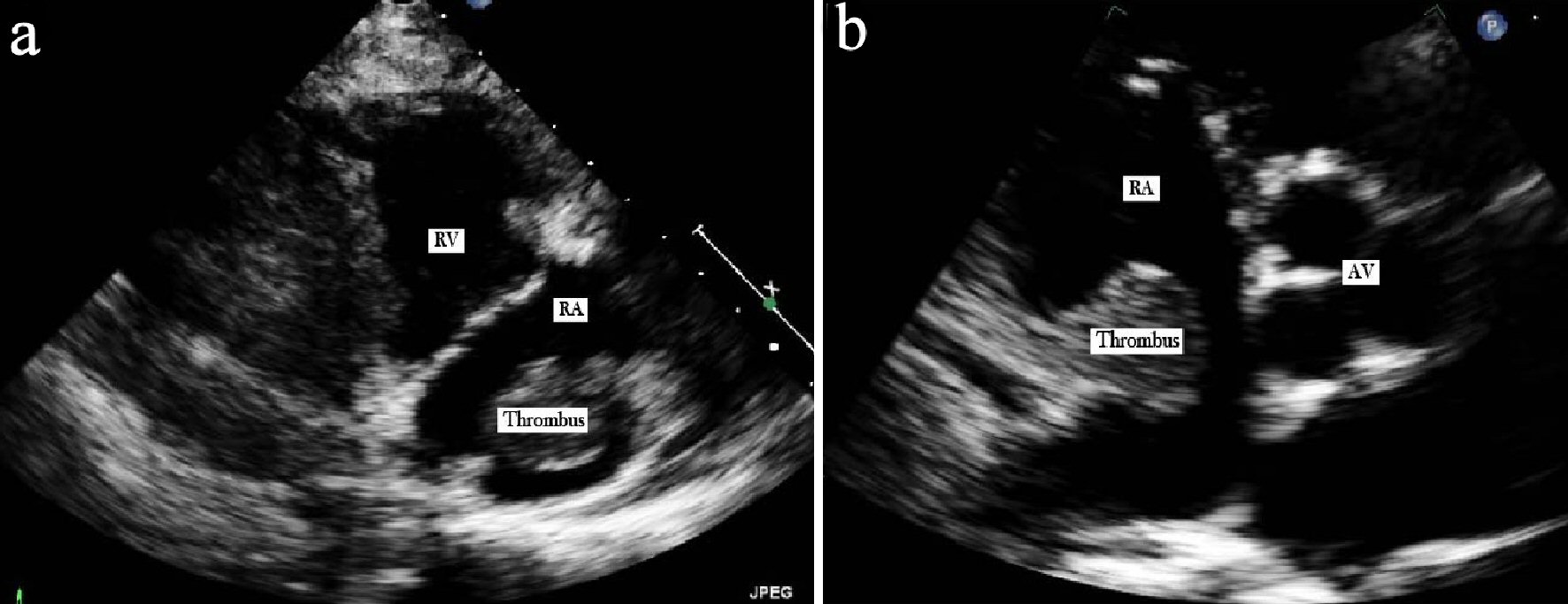 Click for large image | Figure 1. Transthoracic echocardiogram. (a) Parasternal right ventricle inflow view illustrating the RA thrombus. (b) Short axis view showing the RA thrombus attached to the posterior wall through a stalk. |
On arrival, he was hemodynamically stable and asymptomatic. Physical examination was unremarkable. His laboratory findings showed leukocytosis of 15,000 cells/mm3, hemoglobin of 7.5 mg/dL, and a normal platelet count. Computed tomography (CT) imaging showed the RA mass with unclear etiology and other extra-cardiac findings consistent with diffuse HL. A transesophageal echocardiogram (TEE) showed the RA mass attached to the posterior atrial wall and to the central venous catheter (CVC) at the superior vena cava (SVC)/RA junction (Fig. 2). Because there was a question of differentiating between metastatic lesion vs. thrombus, cardiac magnetic resonance imaging (CMR)was also obtained which showed no enhancement of the RA mass with gadolinium contrast injection confirming the diagnosis of CRAT (Fig. 3). Patient was started on heparin for anticoagulation and cardiac thoracic surgery was consulted for possible thrombectomy. During his hospital stay, he developed fever, hypotension and pancytopenia. He was managed in the intensive care unit with broad spectrum antibiotics and vasopressors. Despite aggressive treatment, he rapidly deteriorated and succumbed to the disease.
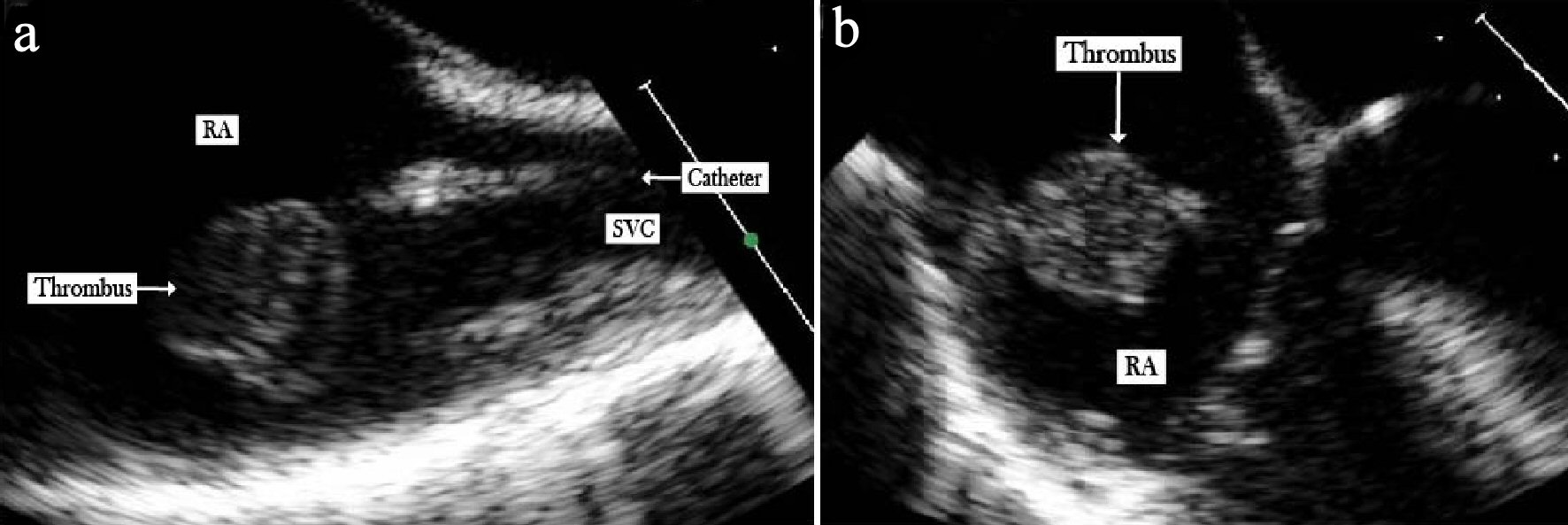 Click for large image | Figure 2. Transesophageal echocardiogram. (a) Bicaval view illustrating the RA thrombus attached to the central venous catheter. (b) Four-chamber view again showing the RA thrombus attached to the posterior wall through a stalk. |
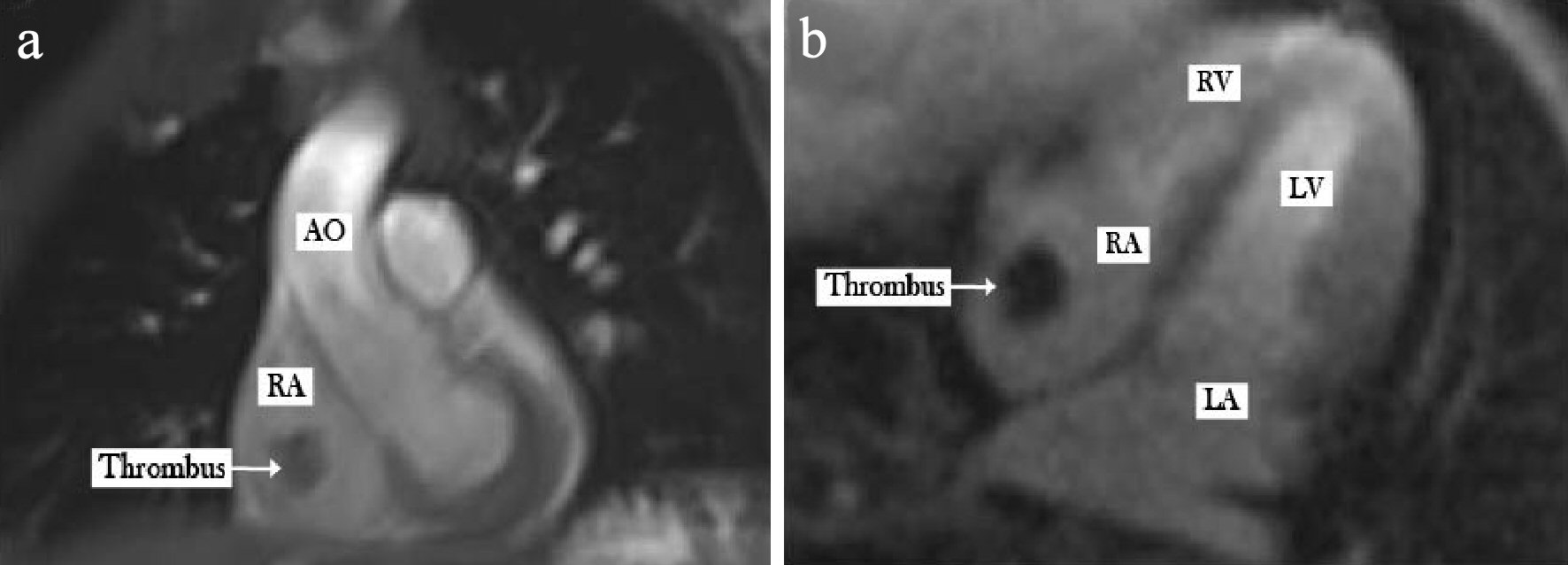 Click for large image | Figure 3. Gadolinium enhanced cardiac magnetic resonance imaging illustrating no uptake by the thrombus. (a) Coronal view. (b) Horizontal long axis view. AO: aorta; RA: right atrium; RV: right ventricle: LA: left atrium: LV: left ventricle; SVC: superior vena cava. |
| Discussion | ▴Top |
In the presence of a RA mass, the differential diagnoses include cardiac or non-cardiac tumors, vegetations, or thrombus formations. Primary cardiac tumors are extremely rare entities with a reported incidence of less than 0.1%. Myxoma is the most common benign cardiac tumor detected. The most common malignant tumor of the heart is from metastatic spread. Majority of the cardiac tumors occupy the left atrium and only 20% appear in the right atrium [2]. Vegetations from infective endocarditis and central venous catheter thrombosis also occur frequently. RA thrombi remain largely underdiagnosed as only one-third of the patients become symptomatic [3]. Catheter-related right atrial thrombi (CRAT) are often seen in patients with indwelling ports for vascular access, as well in patients with long-term intravenous access lines like dialysis catheters.
TTE is the initial diagnostic imaging tool to characterize RA masses. TEE, CT, or CMR are utilized for better tissue characterization and to determine the primary location, site of wall attachment, and overall size [4]. In a cohort of 16 patients, only half of the RA masses found in TEE were described previously in TTE [5]. Due to specific sequencing protocols and superior tissues characterization, CMR has high specificity, showing 95% accuracy in differentiating a tumor from thrombus. A thrombus would appear smaller, less mobile, homogenous, and demonstrate hypointensity in CMR due to their avascularity even after contrast injection. There was no difference between the two entities in T1 weighted MRI images, however hyperintensity in T2 weighted MRI is more commonly seen in tumors [4].
Risk factors for thrombus development include the presence of hypercoagulable states including malignancy, concurrent infection, and renal failure, the presence of the catheter tip at the SVC/RA junction, left-sided or femoral insertion sites, multiple insertion attempts, increased lumen diameter and number of ports, and in peripherally inserted central catheters [3, 6]. Pulmonary embolism (7-11%), septic emboli, cardiac arrhythmias and dysfunction may complicate CRAT [1, 7].
Once diagnosed, a cardiac myxoma undergoes prompt surgical excision while anticoagulation and catheter removal are employed in CRAT [2]. Thrombolysis or surgical thrombectomy is reserved for complicated cases or after the failure of anticoagulation [1, 6]. A review of 177 cases of right heart thromboemboli showed an overall mortality rate of 27.1%. Of those, all patients who did not receive treatment died. Those offered anticoagulation, surgery, or thrombolytic therapy had better mortality rates of 28.6%, 23.8%, and 11.3%, respectively [8]. The prophylactic use of dalteparin in patients with CVCs failed to show a reduction in thromboembolic events [9]. As the use of CVC continues to be widely used, prevention of thrombus formation by avoiding placing the tip of the catheter at the SVC/RA junction, routine TTE in chemotherapy patients, shorter duration of placement, and continuously reassessing the need of CVC should help decrease the incidence of CRAT.
Conclusions
This case highlights the importance of multimodality cardiac imaging in the appropriate diagnosis of a RA mass. Diagnosis of RA mass can be promptly made using multimodal cardiac imaging like TTE, TEE and CMR. CMR has high specificity in differentiating a tumor from thrombus. Even with appropriate treatment, mortality remains high.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Author Contributions
AC and AR wrote and contributed equally to the manuscript. AS and SM edited the content and provided their expertise. All authors read and approved the final version of the manuscript.
Abbreviations
ABVD: adriamycin, bleomycin, vinblastine, dacarbazine; CVC: central venous catheter; CMR: cardiac magnetic resonance imaging; CRAT: Catheter-related right atrial thrombosis; CT: computed tomography; HL: Hodgkin lymphoma; HSCT: hematopoietic stem cell transplant; MRI: magnetic resonance imaging; RA: right atrium; SVC: superior vena cava; TEE: transesophageal echocardiogram; TTE: transthoracic echocardiogram
| References | ▴Top |
- Stavroulopoulos A, Aresti V, Zounis C. Right atrial thrombi complicating haemodialysis catheters. A meta-analysis of reported cases and a proposal of a management algorithm. Nephrol Dial Transplant. 2012;27(7):2936-2944.
doi pubmed - Reynen K. Cardiac myxomas. N Engl J Med. 1995;333(24):1610-1617.
doi pubmed - Gilon D, Schechter D, Rein AJ, Gimmon Z, Or R, Rozenman Y, Slavin S, et al. Right atrial thrombi are related to indwelling central venous catheter position: insights into time course and possible mechanism of formation. Am Heart J. 1998;135(3):457-462.
doi - Pazos-Lopez P, Pozo E, Siqueira ME, Garcia-Lunar I, Cham M, Jacobi A, Macaluso F, et al. Value of CMR for the differential diagnosis of cardiac masses. JACC Cardiovasc Imaging. 2014;7(9):896-905.
doi pubmed - Obeid AI, al Mudamgha A, Smulyan H. Diagnosis of right atrial mass lesions by transesophageal and transthoracic echocardiography. Chest. 1993;103(5):1447-1451.
doi pubmed - Wall C, Moore J, Thachil J. Catheter-related thrombosis: A practical approach. J Intensive Care Soc. 2016;17(2):160-167.
doi pubmed - Kuter DJ. Thrombotic complications of central venous catheters in cancer patients. Oncologist. 2004;9(2):207-216.
doi pubmed - Rose PS, Punjabi NM, Pearse DB. Treatment of right heart thromboemboli. Chest. 2002;121(3):806-814.
doi pubmed - Karthaus M, Kretzschmar A, Kroning H, Biakhov M, Irwin D, Marschner N, Slabber C, et al. Dalteparin for prevention of catheter-related complications in cancer patients with central venous catheters: final results of a double-blind, placebo-controlled phase III trial. Ann Oncol. 2006;17(2):289-296.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


