| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Original Article
Volume 7, Number 1, January 2018, pages 1-6
Alterations of Hematological Parameters, Hemoglobin and Hematocrit With Liver Enzymes, Aspartate Transaminase and Alanine Transaminase Among Patients With Chronic Kidney Disease Undergoing Hemodialysis in Aljouf Region, Saudi Arabia
Mohammad N. Khana, c, Abozer Elderderya, b
aCollege of Applied Medical Science, Aljouf University, Saudi Arabia
bDepartment of Haematology, Faculty of Medicine and Health Sciences, University of El Imam El Mahdi, Sudan
cCorresponding Author: Mohammad N. Khan, Clinical Laboratory Sciences, College of Applied Medical Science, Aljouf University, Saudi Arabia
Manuscript submitted December 14, 2017, accepted December 27, 2017
Short title: Hematological Parameters in CKD
doi: https://doi.org/10.14740/jh367w
| Abstract | ▴Top |
Background: Anemia results from low kidney production of the erythropoiesis-stimulant erythropoietin. Good liver function is crucial to patients with chronic kidney disease (CKD). This study analyzed two hematological parameters (hemoglobin (Hb) and hematocrit (Ht)) and two liver enzymes, alanine aminotransferase (ALT) and aspartate aminotransferase (AST) in patients with CKD undergoing hemodialysis (HD).
Methods: Three hundred and thirty individuals participated in this study. Of them, 159 patients with CKD undergoing HD and 171 healthy individuals as a control group were recruited between January and October 2017. Blood was collected into EDTA containers for complete blood count (CBC) and into additive plain containers for ALT and AST. Relevant case history data were also taken.
Results: Obtained results for first and second month of Hb, Ht, AST and ALT of CKD patients undergoing HD were lower (10.2 g/dL and 8.9 for Hb; 27.2% and 24.8% for Ht; 17.8 IU/L and 15.6 IU/L for ALT; 13.9 IU/L and 12.0 IU/L for AST, respectively) (P < 0.05) compared to healthy individuals (15.1 g/dL for Hb; 44.6% for Ht; 28.3 IU/L for ALT and 23.0 IU/L for AST). Furthermore, Hb, Ht, AST and ALT levels were significantly lower (P < 0.05) in their second month compared to the first month.
Conclusions: Anemia might emerge in CKD patients because of low Hb concentration and consequent low Ht. Advanced stage CKD causes decreased AST and ALT, as a result of lipid metabolism disturbances. Therefore, anemia and liver diseases are recommended to be treated in CKD patients to alleviate related complications. Renal transplantation must be performed earlier for them to avoid further complications.
Keywords: CKD; Hb; Hematocrit; AST; ALT; Liver disease; Aljouf region
| Introduction | ▴Top |
Erythropoietin (EPO) is a hormone made predominantly within the peri-tubular cells of the kidney. This hormone acts on the bone marrow (BM), stimulating erythropoiesis and controlling apoptosis of mature red blood cells (RBCs) [1, 2].
The management of anemia in chronic kidney disease (CKD) has been revolutionized by the development of recombinant human EPO [2, 3]. Many of the symptoms that had been ascribed to CKD such as fatigue, lethargy, somnolence and shortness of breath, which all impact unfavorably on quality of life, were resolved or markedly improved when anemia was corrected [4].
CKD is a prevalent, worldwide condition, and the number of patients affected continues to increase. Diabetes is one of the most common causes of kidney disease [5]. Anemia occurs early in the development of kidney disease and worsens as kidney function deteriorates. Anemia is associated with substantial morbidity and mortality. However, it can be effectively treated, thereby improving the quality of life in patients with CKD and anemia [6].
Patients with CKD undergoing hemodialysis (HD) have lower ALT and AST levels compared to individuals with normal renal function [7, 8]. Deficiency of vitamin B6, a coenzyme of ALT also may cause lower levels of ALT as does hemodilution, which occurs due to water retention in patients with CKD [9, 10].
There has been a proposal to reduce the upper limit of the normal (ULN) of ALT to approximately 70% of the conventional limits while screening for liver abnormalities in patients without CKD [11]. There was in one study an increase in the sensitivity of ALT from 55% to 76% for the diagnosis of discrete liver diseases and specificity was reduced from 97% to 89% when the ULN was reduced [11, 12]. A second study found the risk of mortality from liver disease was higher in individuals with normal levels of ALT that were close to the ULN compared with individuals with lower ALT levels in a large Korean population. A proposal was submitted to reduce the ULN level to 75% of the current ULN level of ALT [13]. In present study, AST and ALT were measured. The hematocrit (Ht) was also assessed to investigate the possibility of hemodilution.
A cross-sectional descriptive, prospective study was first carried out to assess anemia and liver disease in patients with CKD undergoing HD in the Aljouf region of Saudi Arabia. Sakaka city was chosen as the study area because it is the capital city and has a central location in this region.
A great deal of research has been devoted to CKD and control programs are required to minimize the prevalence of this disease. There are no large-scale reports regarding the causes of liver enzymes and hematological parameter alterations among Saudi patients with CKD in the Aljouf region.
The present study was based on a large series of blood samples that were brought from the Prince Motaib General Hospital and analyzed for both hematological parameters and liver enzymes to detect the prevalence of anemia by measuring two hematological parameters, Hb, Ht and the prevalence of liver disease in patients with CKD undergoing HD, by measuring two liver enzymes, alanine aminotransferase (ALT) and aspartate aminotransferase (AST)
| Methods | ▴Top |
The present study was carried out as a case series with an internal comparison group during the period from January to October 2017. It was conducted in the Prince Moteb Bin Abdulaziz Hospital, Aljouf and Hematology Lab, Faculty of Applied Medical Sciences, Aljouf University. One hundred and fifty-nine patients with CKD undergoing HD who were admitted to the Prince Moteb Bin Abdulaziz Hospital and 171 healthy individuals of Sakaka city were recruited to participate in this study (330 participants in total).
In this study, a no-probability sample equation (n = N/1 + N (e) 2) was used to determine sample size [14], but for feasibility reasons, only 150 - 170 samples for patients and 150 - 180 for healthy individuals were chosen.
Self-administered questionnaire was designed to obtain information which was used in the study. Histories of disease, date of dialysis, frequency, etc. were also taken. Selected individuals were informed with detailed objectives of the study and its importance for the future. All information obtained from patient specimens and results were kept as highly security data. The participants were provided with information about the study and any risk that may arise especially during specimen collection. Ethical approval was obtained from the relevant authorities (Aljouf University, College of Applied Medical Sciences and the above mentioned Teaching Hospital).
Hematological parameters (Hb and Ht) and liver enzymes (ALT and AST) were measured for all study participants. Blood samples from patients with CKD undergoing HD and healthy individuals were collected into two blood containers, an EDTA container for hematological parameters, using hematolgy analyzer (Sysmex) and an additive plain container for liver enzymes, using the chemistry analyzer, Dimension-200 EXL, Siemens.
Data were analyzed with graphs and tables created using SPSS™. Descriptive statistics were given for some variables such as Hb, Ht, ALT, AST and Student’s t-test was employed to detect significant differences (see results).
Base-line characteristics included liver enzymes and hematological parameters. These results were compared with samples from patients and healthy individuals according to the above parameters.
| Results | ▴Top |
Obtained results for first and second month of Hb, Ht, AST and ALT are expressed in Table 1. Of these, the control (healthy individuals) results were within published normal ranges.
 Click to view | Table 1. Results of Hb, Hematocrit, ALT and AST of the First and Second Month of Patients With CKD Undergoing Hemodialysis Versus Healthy Individuals |
Obtained results for first and second month of hematological parameters, Hb and Ht of CKD patients undergoing HD were lower (10.2 g/dL and 8.9 g/dL for Hb; 27.2% and 24.8% for Ht) (P < 0.05) compared to healthy individuals (15.1 g/dL for Hb; 44.6% for Ht). Furthermore, Hb and Ht levels were significantly lower (P < 0.05) in their second month compared to the first month, as shown in Table 1 and Figure 1.
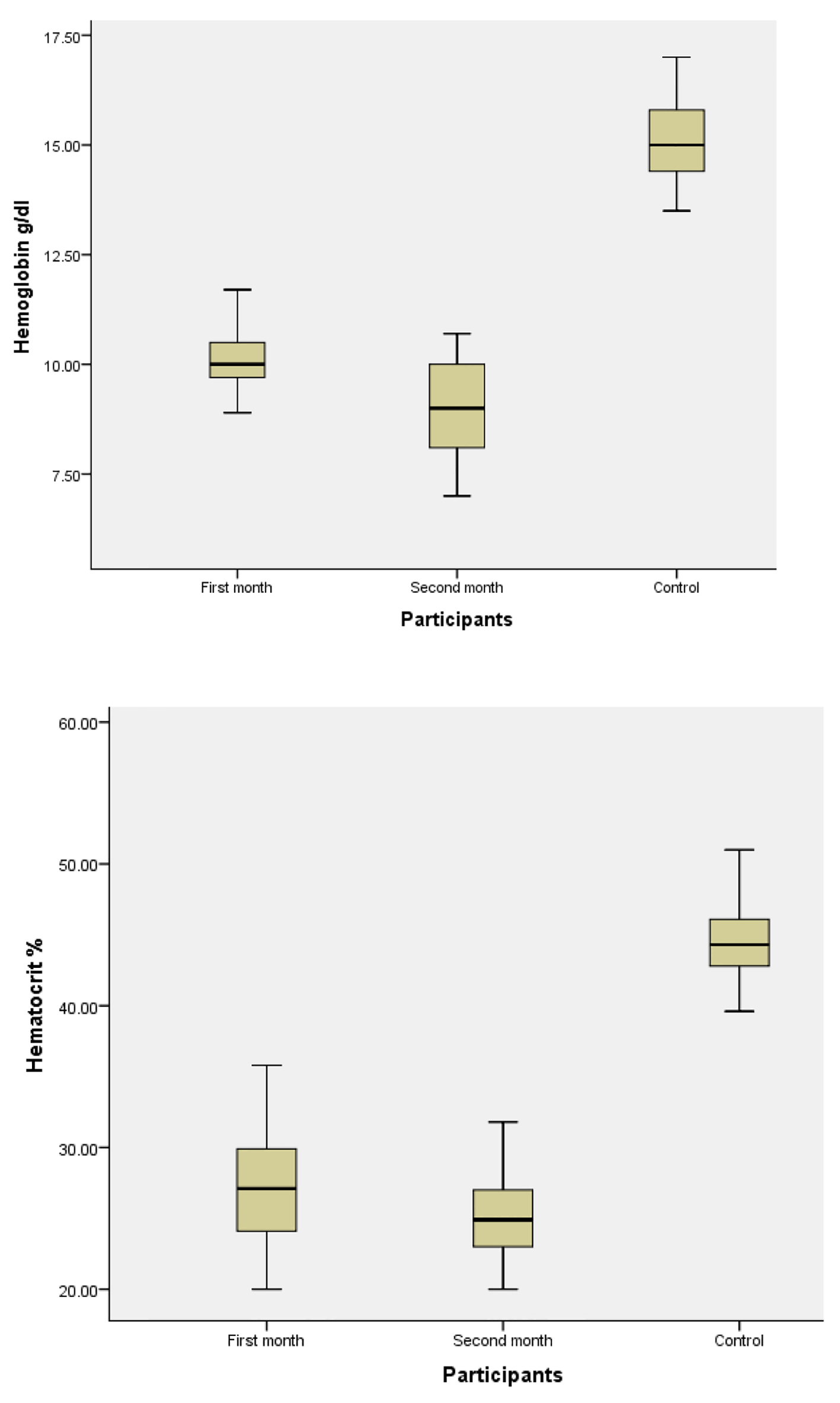 Click for large image | Figure 1. Hemoglobin and hematocrit level in study population. |
Obtained results for first and second month of liver enzymes, AST and ALT of CKD patients undergoing HD were lower (17.8 IU/L and 15.6 IU/L for ALT; 13.9 IU/L and 12.0 IU/L for AST) (P < 0.05) compared to healthy individuals (28.3 IU/L for ALT and 23.0 IU/L for AST). Moreover, AST and ALT levels were significantly lower (P < 0.05) in their second month compared to the first month, as depicted in Table 1 and Figure 2.
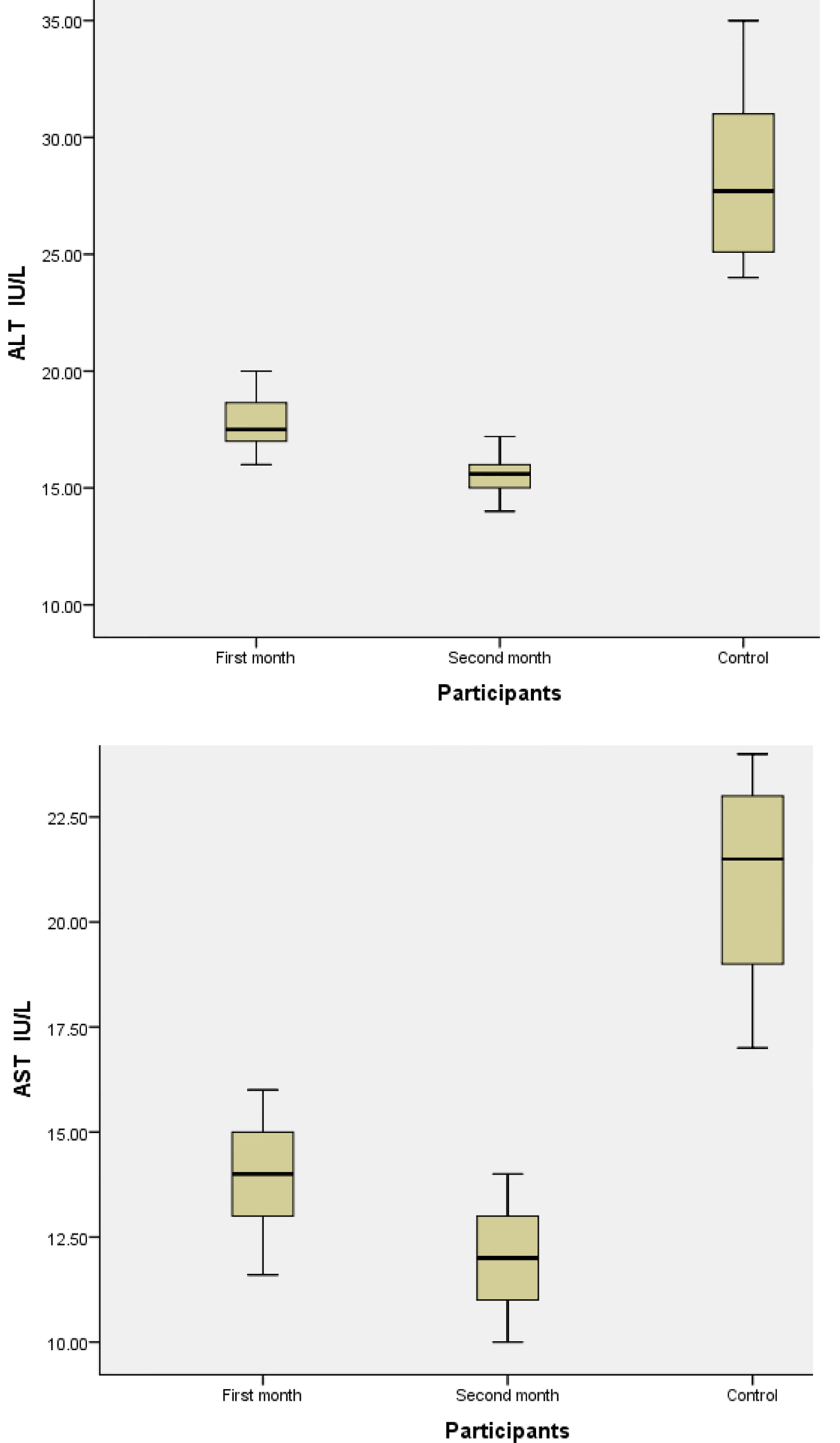 Click for large image | Figure 2. ALT and AST among study population. |
| Discussion | ▴Top |
This cross-sectional descriptive, prospective study was first carried out in the Aljouf area to determine the occurrence of anemia and liver disease in patients with CKD undergoing HD at Sakaka city, Aljouf region, by measuring two hematological parameters, Hb, Ht and liver enzymes, ALT and AST.
This work may act as a pilot study for further research, because of less available published data regarding the alterations in Hb, Ht, ALT and AST among Saudi patients with CKD undergoing HD in the Aljouf region.
Anemia is defined by the World Health Organization (WHO) as a low Hb concentration, below 13.0 g/dL for adult males and below 12.0 g/dL for adult females [15]. By these criteria, almost all of our patients with CKD undergoing HD had anemia (Table 1). This finding is in agreement with similar studies [16-18], and this is due to less erythropoietin being produced by the diseased kidneys [19].
Of patients with CKD undergoing HD in the current study, Hb and Ht levels were significantly lower in the first and second month (10.2 g/dL and 8.9 g/dL for Hb; 27.2% and 24.8% for Ht) (P < 0.05) compared to healthy individuals (15.1 g/dL for Hb; 44.6% for Ht). Furthermore, Hb and Ht levels were significantly lower (P < 0.05) in their second month compared to the first month, as shown in Table 1 and Figure 1. This means that anemia is getting worse with time in these patients and consequently high morbidity and mortality might occur in patients with CKD undergoing HD if they are not prevented from becoming anemic. Therefore, a renal anemia management period (RAMP) protocol is suggested to call attention to the need to improve outcomes for patients with CKD undergoing HD and probably reduce the economic burden by correcting anemia early on.
Obtained results for first and second month of liver enzymes, AST and ALT of CKD patients undergoing HD were lower (17.8 IU/L and 15.6 IU/L for ALT; 13.9 IU/L and 12.0 IU/L for AST) (P < 0.05) compared to healthy individuals (28.3 IU/L for ALT and 23.0 IU/L for AST). Moreover, AST and ALT levels were significantly lower (P < 0.05) in their second month compared to the first month, as demonstrated in Table 1 and Figure 2. A study was hypothesized that this decrease might be due to the occurrence of uremic factors which may constrain the activity of AST and ALT enzymes [20], and finally, deficiency in pyridoxine, a cofactor for the production of the aminotransferases.
Additionally, the high lactate serum levels during biochemical dosages might quickly consume nicotinamide adenine dinucleotide phosphate (NADPH) and therefore reduce the levels of aminotransferases. Serum aminotransferases are reduced in patients with CKD on HD as hemodilution is involved in this reduction. Other factors, such as pyridoxine deficiency or elevated homocysteine, may also be involved in lowering aminotransferases.
Conclusions
A great deal of research elsewhere has been devoted to CKD and control programs are required to minimize the prevalence of this disease, because it is accompanied with serious complications including some clinical conditions, for instance liver diseases and anemia. Therefore renal transplantation is suggested to be considered for patients with CKD rather than continuing on doing HD for them, which might assist those patients in not having further complications such as anemia and liver diseases.
Acknowledgments
The authors thank individuals for their participation. We would like to thank our colleagues at hematology and clinical biochemistry departments. We would also like to thank staff and administration of Prince Motib Bin Abdelaziz hospital for their cooperation. The authors are thankful to the Deanship of Scientific Research and postgraduate studies, Aljouf University for funding the work through the research group project No. 3/38/12682.
| References | ▴Top |
- Khodosovskii MN, Zinchuk VV. [Erythropoietin influence on the blood oxygen transport and prooxidant-antioxidant state during hepatic ischemia-reperfusion]. Ross Fiziol Zh Im I M Sechenova. 2014;100(5):592-601.
pubmed - Mudge D, Webster A. Erythropoiesis-stimulating agents for anaemia in chronic kidney disease: Are they all the same? Cochrane Database Syst Rev. 2014;12:ED000093.
doi - Hung SC, Kuo KL, Tarng DC, Hsu CC, Wu MS, Huang TP. Anaemia management in patients with chronic kidney disease: Taiwan practice guidelines. Nephrology (Carlton). 2014;19(12):735-739.
doi pubmed - Cases-Amenos A, Martinez-Castelao A, Fort-Ros J, Bonal-Bastons J, Ruiz MP, Valles-Prats M, Coll-Piera E, et al. Prevalence of anaemia and its clinical management in patients with stages 3-5 chronic kidney disease not on dialysis in Catalonia: MICENAS I study. Nefrologia. 2014;34(2):189-198.
pubmed - Silverberg DS, Wexler D, Iaina A, Schwartz D. The correction of anemia in patients with the combination of chronic kidney disease and congestive heart failure may prevent progression of both conditions. Clin Exp Nephrol. 2009;13(2):101-106.
doi pubmed - Cook JR, Dillie KS, Hakeem A, Bhatti S, Chang SM. Effectiveness of anemia and chronic kidney disease as predictors for presence and severity of coronary artery disease in patients undergoing stress myocardial perfusion study. Am J Cardiol. 2008;102(3):266-271.
doi pubmed - Fabrizi F, Lunghi G, Ganeshan SV, Martin P, Messa P. Hepatitis C virus infection and the dialysis patient. Semin Dial. 2007;20(5):416-422.
doi pubmed - Alberti A, Noventa F, Benvegnu L, Boccato S, Gatta A. Prevalence of liver disease in a population of asymptomatic persons with hepatitis C virus infection. Ann Intern Med. 2002;137(12):961-964.
doi pubmed - Fabrizi F, Lunghi G, Finazzi S, Colucci P, Pagano A, Ponticelli C, Locatelli F. Decreased serum aminotransferase activity in patients with chronic renal failure: impact on the detection of viral hepatitis. Am J Kidney Dis. 2001;38(5):1009-1015.
doi pubmed - Lopes EP, Sette LH, Sette JB, Luna CF, Andrade AM, Moraes M, Sette PC, et al. Serum alanine aminotransferase levels, hematocrit rate and body weight correlations before and after hemodialysis session. Clinics (Sao Paulo). 2009;64(10):941-945.
doi pubmed - Sette LH, Almeida Lopes EP. Liver enzymes serum levels in patients with chronic kidney disease on hemodialysis: a comprehensive review. Clinics (Sao Paulo). 2014;69(4):271-278.
doi - Liberato IR, Lopes EP, Cavalcante MA, Pinto TC, Moura IF, Loureiro Junior L. Liver enzymes in patients with chronic kidney disease undergoing peritoneal dialysis and hemodialysis. Clinics (Sao Paulo). 2012;67(2):131-134.
doi - Kim HC, Nam CM, Jee SH, Han KH, Oh DK, Suh I. Normal serum aminotransferase concentration and risk of mortality from liver diseases: prospective cohort study. BMJ. 2004;328(7446):983.
doi pubmed - Gardi JE, Nyengaard JR, Gundersen HJ. The proportionator: unbiased stereological estimation using biased automatic image analysis and non-uniform probability proportional to size sampling. Comput Biol Med. 2008;38(3):313-328.
doi pubmed - Organization. WH. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity World Health Organization. 2102.
- Nasri H. Renal Cell Protection of erythropoietin beyond correcting the anemia in chronic kidney disease patients. Cell J. 2014;15(4):378-380.
pubmed - Nasri H, Ghorbani A. Does erythropoietin slow progression of chronic kidney disease? J Renal Inj Prev. 2013;2(2):81-82.
pubmed - Noce A, Dessi M, Durante O, Manca di Villahermosa S, Canale MP, Di Daniele N. Influence of continuous erythropoietin receptor activator on markers of cardiovascular risk in chronic kidney disease patients. Int J Cardiol. 2013;167(6):3070-3072.
doi pubmed - Erslev AJ, Besarab A. Erythropoietin in the pathogenesis and treatment of the anemia of chronic renal failure. Kidney Int. 1997;51(3):622-630.
doi - Candinas D, Keusch G, Schlumpf R, Burger HR, Gmur J, Largiader F. [Hemolytic-uremic syndrome following kidney transplantation: prognostic factors]. Schweiz Med Wochenschr. 1994;124(41):1789-1799.
pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


