| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Case Report
Volume 7, Number 1, January 2018, pages 23-28
Follicular Lymphomas of Oral Region Treated by Rituximab Monotherapy: About Two Cases
Sylvain Montanera, b, Noelle Weingertnerc, Marie-Pierre Ledouxd, e, Marie-Pierre Chenardc, e, Jean-Christophe Lutze, f, g, Fabien Bornerta, b, g, h
aDental Faculty, University of Strasbourg, 8 rue Sainte Elisabeth, F-67000 Strasbourg, France
bOral Surgery and Oral Medecine Unit, Dental Clinic, Hopital Civil, University Hospital of Strasbourg, 1 place de l’Hopital, F-67000 Strasbourg, France
cDepartment of Pathology, Hopital de Hautepierre, University Hospital of Strasbourg, 1 avenue Moliere, F-67000 Strasbourg, France
dDepartment of Hematology, Hopital de Hautepierre, University Hospital of Strasbourg, 1 avenue Moliere, F-67000 Strasbourg, France
eFaculty of Medicine, University of Strasbourg, 4 rue Kirschleger, F-67000 Strasbourg, France
fStomatology Maxillo-Facial and Plastic Surgery Department, Hopital Civil, University Hospital of Strasbourg, 1 place de l’Hopital, F-67000 Strasbourg, France
gINSERM (French National Institute of Health and Medical Research), “Osteoarticular and Dental Regenerative Nanomedicine” Laboratory, UMR 1109, Faculte de Medecine, FMTS, F-67085 Strasbourg Cedex, France
hCorresponding Author: Fabien Bornert, Unite de Pathologie-Chirurgie Buccale, Pole de Medecine et de Chirurgie Bucco-Dentaires, Hopital Civil, Hopitaux Universitaires de Strasbourg, 1 place de l’Hopital, 67000 Strasbourg, France
Manuscript submitted October 3, 2017, accepted October 23, 2017
Short title: Follicular Lymphomas of Oral Region
doi: https://doi.org/10.14740/jh346w
| Abstract | ▴Top |
Lymphomas represent the second most common malignant lesions of the head and neck. Among them, follicular lymphomas (FLs) are the second most frequent B-cell non-Hodgkin’s lymphomas. However, their incidence is rare in the oral cavity. We describe here two cases of FL with initial intra-oral presentation. The first patient was 81 years old and presented a palatal hyperplasia, covering the posterior edge of her dental removable prosthesis. After surgical excision of the lesion, the pathological diagnosis was an extra-nodal low-grade follicular lymphoma. Medical imaging assessment found a widespread but non-bulky involvement. The second patient was 38 years old and referred for asymptomatic swelling of the lower vestibule evolving for 4 months. Surgical exploration revealed a cheek lymphadenopathy infiltrated by a grade 3 FL; this patient did not have any other localization. Both patients were treated by a rituximab monotherapy with excellent response after 2 years of follow-up. Most of the time, FL affecting the oral cavity presenting as unspecific swelling, can mimic other frequent and benign oral lesions. In the absence of biopsy, both diagnosis and proper onco-hematological management may be delayed. The introduction of monoclonal antibody rituximab represents a major advance in the management of FL: it can be used as monotherapy or may be combined with chemo-immunotherapy according to histological grading, initial staging (extent, tumor mass or bulk), age and co-morbidities. These two observations show the importance of an early diagnosis regarding a chronic lesion in the oral cavity. Painless lymphadenopathy, asymptomatic swelling, aspecific mucosal lesions, or subprosthetic lesions should draw attention of any oral specialist.
Keywords: Follicular lymphoma; Oral cavity; Rituximab; Nodal and extra-nodal presentation
| Introduction | ▴Top |
Even though lymphomas represent approximately 5% of malignant neoplasm of the head and neck region, they are the second most common malignant lesions after the squamous cell carcinoma [1, 2]. These lymphomas mainly consist of non-Hodgkin’s lymphomas (NHLs). They are a heterogeneous group of disease defined by an abnormal proliferation of lymphoid cells, affecting the B lineage in 85% of cases. Most of these lymphomas occur in the Waldeyer ring [3]. Occurrence of lymphoma in the oral cavity is relatively rare, accounting for approximately 3.5% of oral malignancies [4]. Diffuse large B-cell lymphoma (DLCBL) is the most common form, followed by follicular lymphoma (FL) [2]. Extranodal marginal zone lymphoma of the mucosa-associated lymphoid tissue (MALT) is also frequent in the oral and maxillofacial region. Other rare subtypes can be found, such as chronic lymphocytic leukemia, nodal marginal zone lymphoma, mantle cell lymphoma, Burkitt lymphoma and T-cell lymphoma [5]. FL is a non-Hodgkin lymphoma affecting the B phenotype classified in four histological subtypes (1, 2, 3A, and 3B). They feature indolent behavior, especially for grades 1 and 2, few clinical symptoms and a slow evolution [6]. Only grade 3B FL shall be considered as an aggressive form. Because of its rare incidence in the oral cavity and its non-specific clinical forms, FL diagnosis is a challenge. We describe two cases of FL, initially presenting as common oral cavity lesions, but finally featuring a rather different staging.
| Case Reports | ▴Top |
Case 1
An 81-year-old female patient was referred by her dentist for teeth extractions and evaluation of a palatal swelling (Fig. 1). The patient’s medical record included post-hypertensive and valvular cardiomyopathy, chronic kidney failure and chronic obstructive pulmonary disease. Clinical examination found a painless palatal hyperplasia covering the posterior edge of a dental prosthesis. This hyperplasia consisted of a sessile lesion with an overlying mucosa devoid of any ulceration or inflammation (Fig. 1).
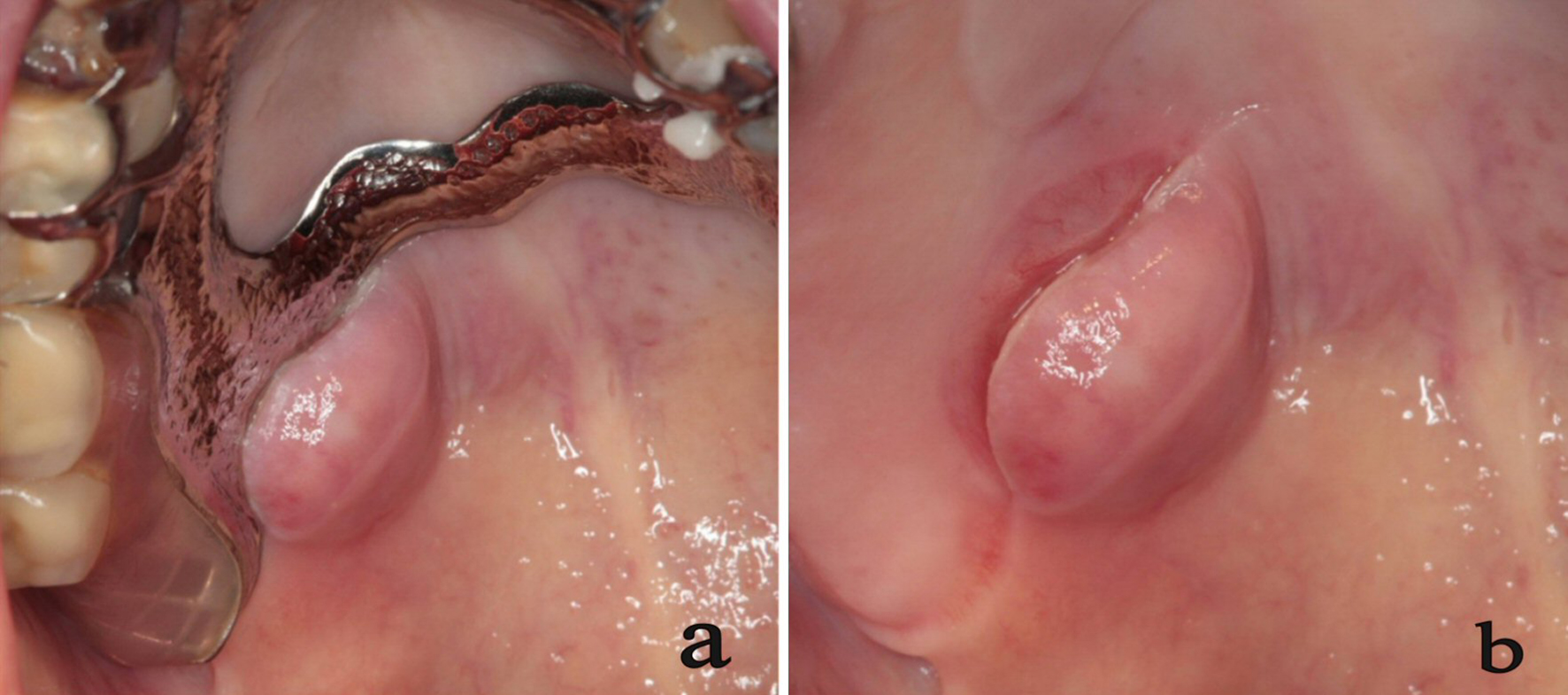 Click for large image | Figure 1. Intra-oral view. Clinical views of the lesion with (a) and without (b) the removable prosthesis. These views show a nodulary sessile mass on soft palate with inflammatory aspect on the surface and related to the prosthetic edge. |
An excisional biopsy was immediately performed under local anesthesia. Histopathological analysis showed a lymphoid proliferation arranged in follicular architecture. This lymphoid proliferation was represented by small-sized lymphoid cells (centrocytes) combined with some bigger cells (10 - 15 centroblasts by field of view with × 40 magnification) (Fig. 2a, b).
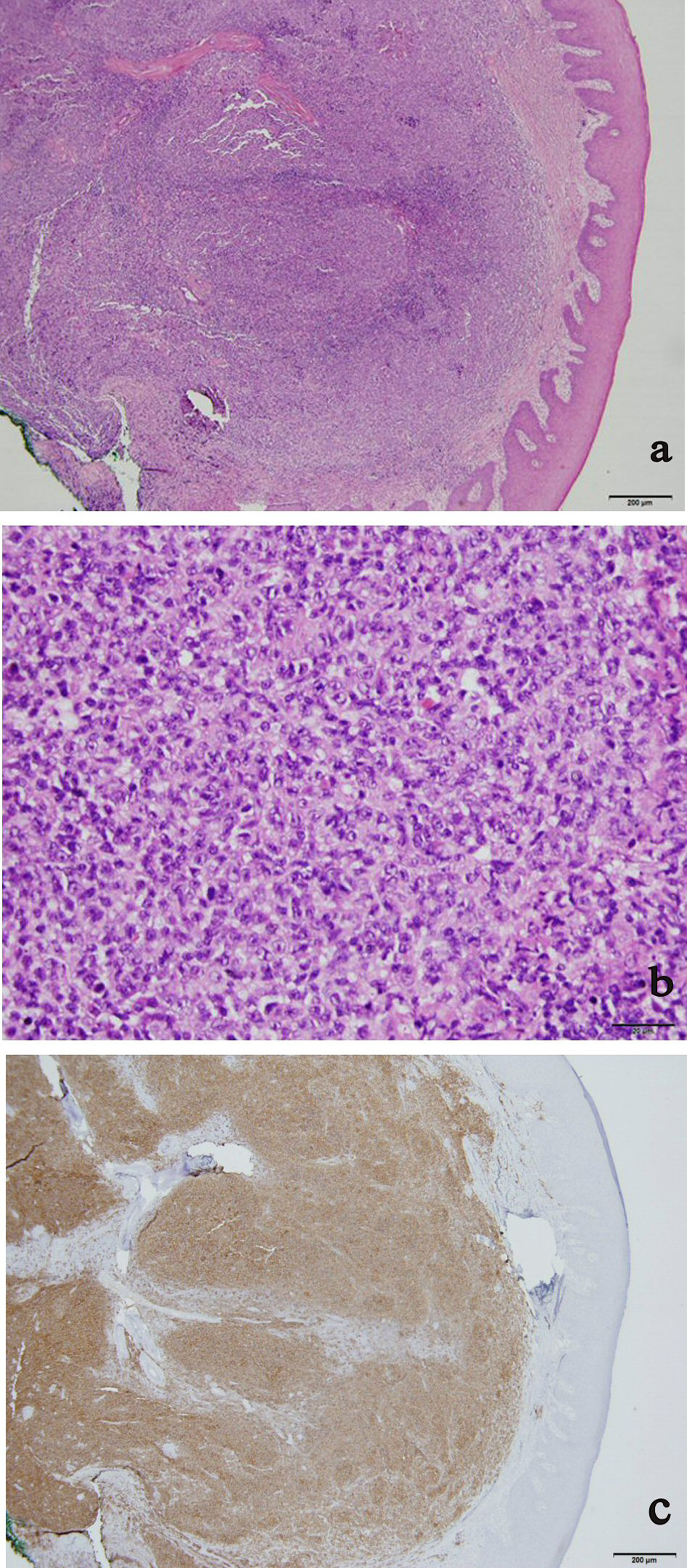 Click for large image | Figure 2. Microscopical views. Slides 2a (hematoxylin-eosin staining (HE), × 4) and 2b (HE, × 40) showing proliferation of lymphoid cells of small sizes (centrocytes) and of 10 to 15 of big sizes cells (centroblast) by field of view organized in follicular architecture and without tangible body macrophages; oral mucosa is covered by a normal malpighian epithelium; slide 2c (immunochemistry, × 4) shows a strong positivity to CD20 antibody compatible with B cells infiltration. |
Immunostaining was positive for cluster designation 20 (CD20), therefore confirming the B nature of this tumoral proliferation (Fig. 2c). It was also positive for CD10, bcl-6, and bcl2. The CD23 immunostaining highlighted a dissociated meshwork of follicular dendritic cells. The Ki67 proliferation index was low (30%) (Table 1).
 Click to view | Table 1. Immunohistochemical Pattern |
The diagnosis of grade 2 follicular lymphoma was established.
Medical imaging assessment (positron emission tomography (PET) scan and cervico-thoraco-abdominal-pelvic computed tomography (CT) scan) revealed multiple small-sized involved lympadenopathies corresponding to Ann Harbor stage IV (Fig. 3).
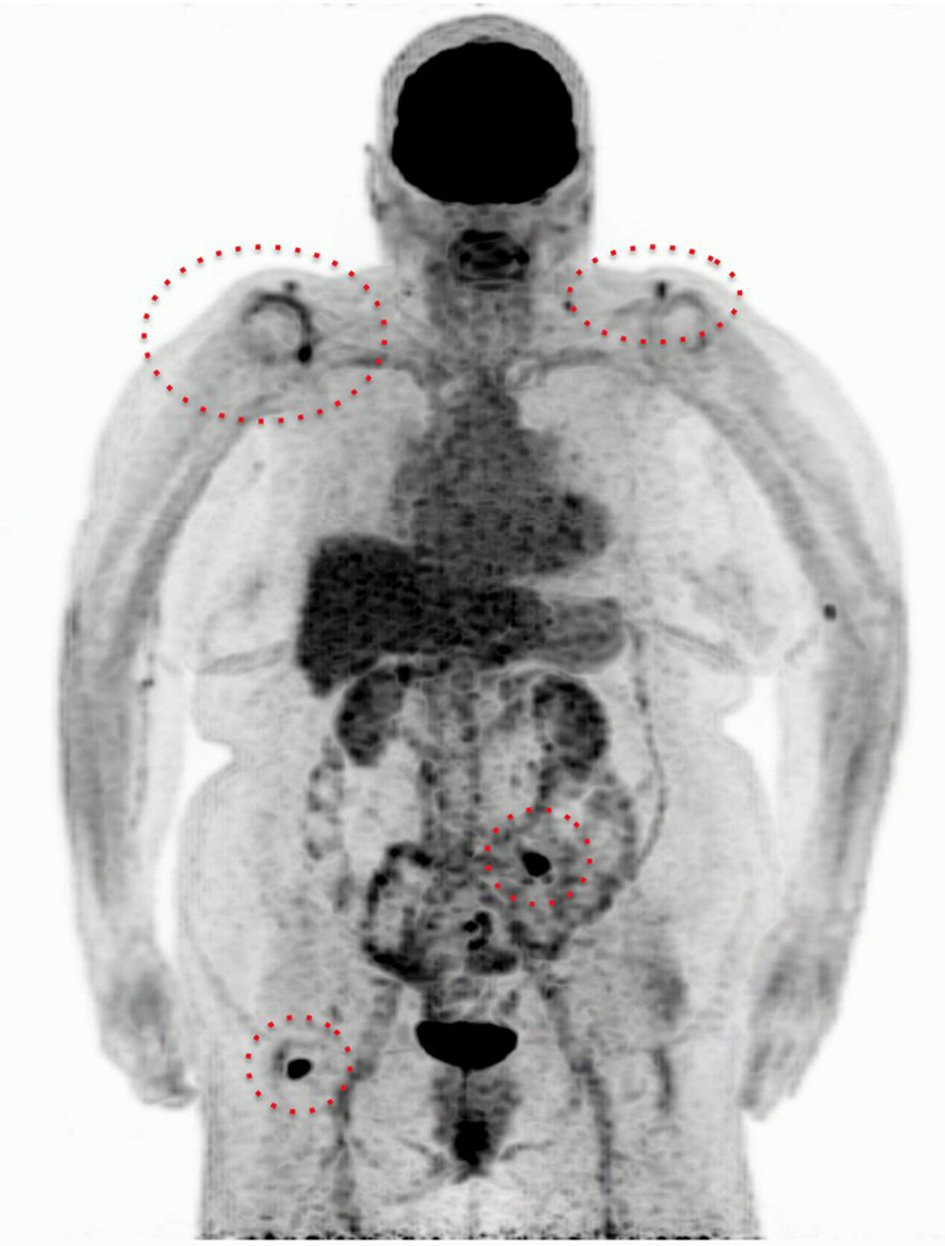 Click for large image | Figure 3. The 18-FDG PET-scanner of case 1. In cephalic region, we note a focal hyperfixation into the right palate which can correspond to a post-operative inflammation. In the thoraco-abdomino-pelvic region, there are two clavicular, one mesenteric and one right inguinal nodes. |
Blood test showed low hemoglobin, an increase in the β2 microglobulin level, as well as an increase in the lactate dehydrogenase level. Therefore, according to the FILIPI-1 prognosis index, the patient belonged to a high-risk group.
Considering the patient’s medical condition, the extended stage and the low proliferation index without bulky disease, a monoclonal anti-CD20 antibody monotherapy (rituximab, 375 mg/m2 IV weekly) was initiated. No side effect was noted. Maintenance therapy every 3 months was then delivered for three additional cycles with an overall 10 months treatment. Imaging follow-up, consisting of PET CT and CT scan at 1 year, showed an important regression of mesenteric lymph node infiltration and the absence of evolutive lesions. No disease progression was observed after more than 2 years of follow-up. However, the patient died at the age of 84 years, due to her cardiovascular diseases.
Case 2
A 38-year-old woman was referred by her general practitioner for an asymptomatic swelling in the lower left vestibule evolving for about 4 months. Her dentist initially suspected a dental infection leading to the endodontic treatment of the first left lower molar (Fig. 4a). The overlying mucosa had a healthy appearance and palpation revealed a submucosal mass of elongated shape and firm consistency (Fig. 4b).
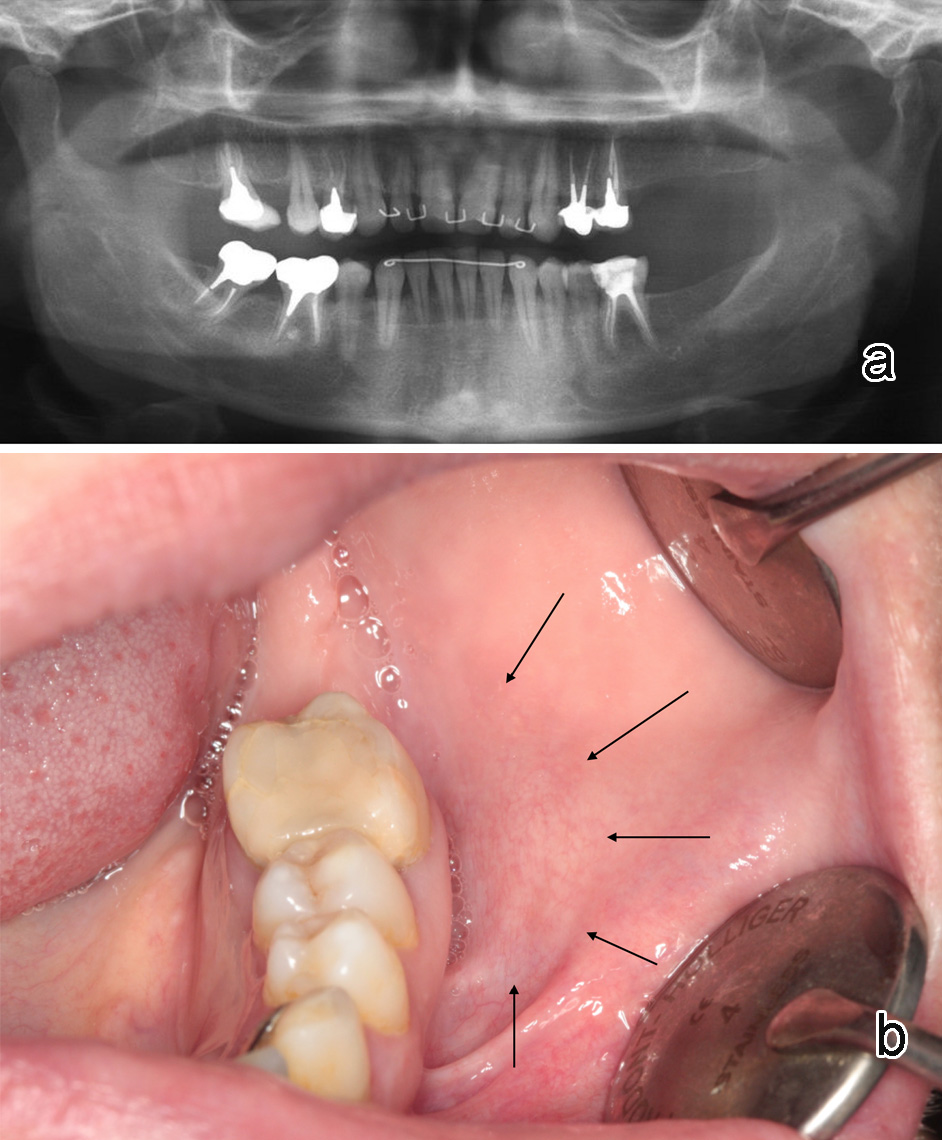 Click for large image | Figure 4. Clinical and radiological presentation of case 2. No dental infection in relation to buccal swelling (b) is observed on panoramic X-ray (a). |
MRI requested by her general practitioner found an encapsulated tissue mass that was in close relation to the external cortex of the mandible, extending from tooth 34 to 37 (Fig. 5).
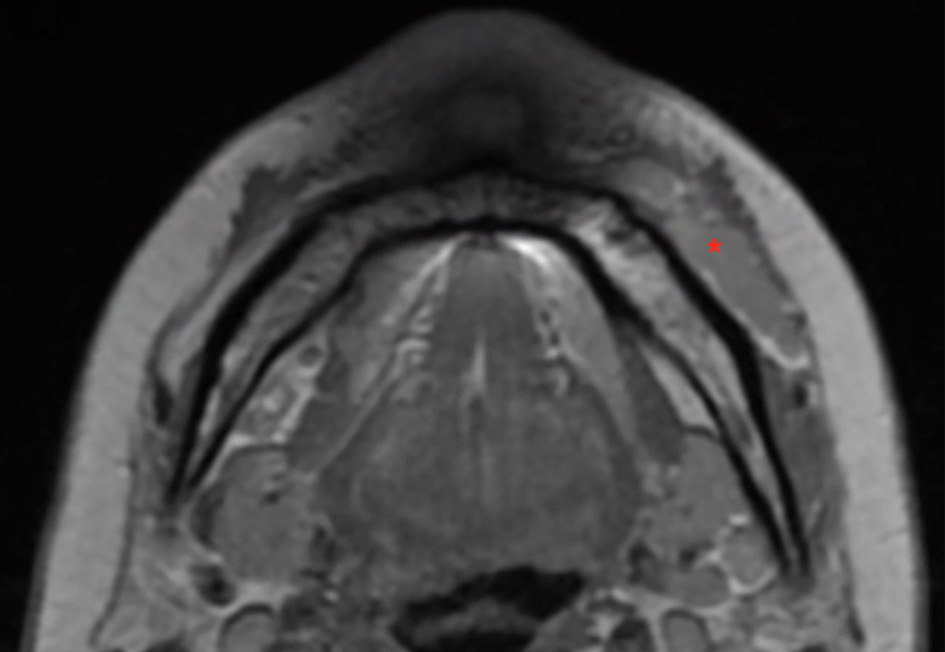 Click for large image | Figure 5. Facial magnetic resonance imaging (MRI) of case 2. Axial slice through mandibular body showing an elongated and well limited mass (*) slightly enhanced by gadolinium in T1 weighted image and laying in the buccal corridor against the buccal cortex. |
Surgical exploration was performed through an oral approach under local anesthesia. It was found that a yellowish lympadenopathy laying under the buccinator muscle; an incisional biopsy of the lesion was performed.
Histopathological examination revealed a grade 3B follicular lymphoma (Fig. 6). The immunohistochemical profile found positivity for CD20 and bcl6, low positivity for CD10 and negativity for bcl2. The CD23 immunostaining also highlighted a dissociated meshwork of follicular dendritic cells. The Ki67 proliferation index was 70% (Table 1).
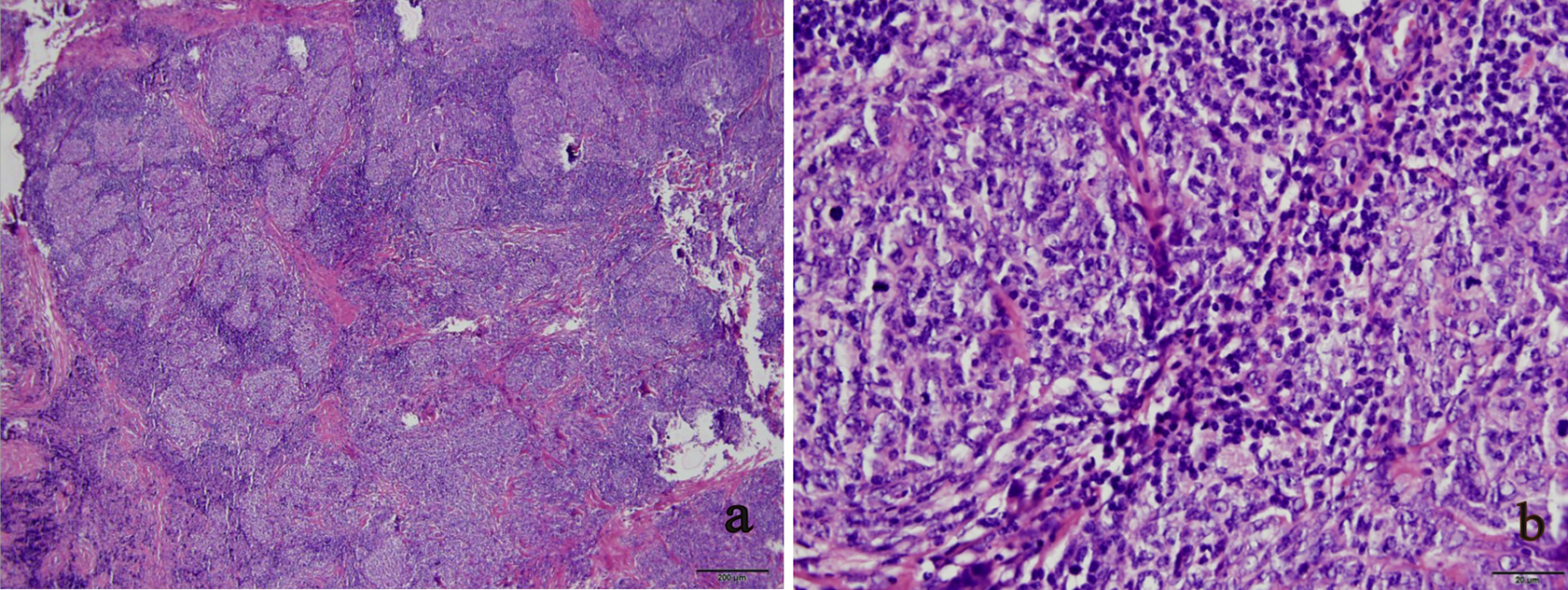 Click for large image | Figure 6. Microscopical views of case 2. (a) Lymphoid proliferation clustered into identifiable nodules (HE, × 4). (b) Centroblast cells are mainly observed in the field of view with many mitoses (HE, × 40). |
PET CT only found hyperfixation in the left cheek 6 weeks after biopsy, probably due to inflammation.
The blood test did not show any abnormalities.
Rituximab (375 mg/m2 IV weekly) was administrated during the first month and the patient was further treated with six intra-venously maintenance cycles every other month for a total duration of 1 year. It allowed complete tumor regression. The patient remained in complete remission for more than 30 months of follow-up after diagnosis.
| Discussion | ▴Top |
FL represents 20 to 25 percent of all lymphomas and over 70% of “low malignancy grade” or “indolent” lymphomas [6]. In a study by Argyris et al including 92 NHL located in the oral cavity, 8.7% were diagnosed as FL [7].
Most of the patients have a widely spread disease at time of diagnosis [8]. Clinical presentation of FL consists of a nodal disease with, in the majority of cases, multiple lymph node enlargements [6]. Nevertheless, in the oral cavity, lymphomas are usually extra-nodal in 40 % of cases according to Jordan et al [9], as in case 1. A primitive oral manifestation is found in only 2% of extra-nodal NHL [10]. In the oral cavity, the most common site of involvement is the palate but NHL may involve both, osseous and soft tissues [11]. Therefore, initial diagnosis of oral lymphoma can be difficult. Just like in our observations, most of NHL is hardly ever accompanied by “B symptoms” such as weight loss, unexplained fever, or night sweats [3]. In the oral cavity, NHL commonly presents as asymptomatic, localized or diffuse, soft tissue swelling [12]. A superficial ulceration of the tumor mass is often encountered [11]. Differential diagnosis in the oral cavity includes squamous cell carcinoma, tumors of minor salivary glands and benign lymphoproliferative disease (e.g. follicular lymphoid hyperplasia) [11]. The lesions can also result from inflammatory (reaction hyperplasia [13]) or infective odontogenic or periodontal conditions (non-healing socket, pyogenic granulomas [14, 15]). Such conditions can lead to inadequate therapeutics (root canal therapy, extractions, antimicrobial chemotherapy) and delayed diagnosis [11]. Fourteen percent of patients may have pain [11]. Misdiagnosis of periapical inflammatory disease can then be more frequent especially when radiolucient osteolysis is observed [14]. Radiologic findings of NHL are not specific: they commonly exhibit diffuse bone destruction, appear as a solitary defect or a lowering of the alveolar bone margin. They can even lead to a condition resembling periodontitis or periodontal abscesses [11]. In a systematic literature review of the oral manifestations of lymphomas, Silva et al report that about 40 % were initially misdiagnosed as a different pathology and were treated as such. It resulted in delayed proper treatment, therefore allowing the progression of the lymphoma [4].
In our first case, the palatal hyperplasia overlying the removable prosthesis could also have been misdiagnosed as a fibro-epithelial polyp or a reactive hyperplasia. In our second case, the patient was referred for a second medical advice after 4 months. A chronic apical periodontitis of 36 was initially diagnosed as the origin of the cheek’s swelling.
Diagnosis of FL includes histopathological and immunohistochemical criteria. Some genetical investigations can be conducted in cases of difficult diagnosis. A full excisional lymphadenopathy biopsy is preferable for proper analysis. Microscopical views show small-sized cells (centrocytes) associated in different proportions to large-sized cells (centroblasts) and arranged in a follicular pattern with a meshwork of dendritic cells. Mitotic activity is proportional to the presence of large cells. WHO staging is based on 3 grades: grade 1 with zero to five centroblasts, grade 2 with six to 15 centroblasts, grade 3 with more than 15 centroblasts by field of view (× 40 magnification). Grade 3 is divided into two subtypes: grade 3A with persistence of some centrocytes and grade 3B with centroblasts only, which are considered as DLCBL. Immunophenotyping shows positivity to CD20, CD10 and bcl6. The proliferation index is also correlated to the staging with a rate superior to 20% for grades 3. The blc2 protein is expressed by cells in 90% of grades 1-2 and in 50% of grade 3 cases. Cells can variably express CD23 or CD43, but not CD5 [6, 7].
Transformation of FL to a higher grade lymphoma, usually DLCBL, is encountered in about 40% of cases [15]. The mean survival after first diagnosis ranges from 17 months in patients presenting with DLCBL to 8.5 years in patients with FL [2].
FL grades 1, 2, and 3A should be considered as an indolent disease. Stage of dissemination, criteria for “bulky” tumor mass, as well as age and co-morbidities, determine the choice for different treatment options. These options range from a “wait-and-watch” approach for localized small masses (since progression may be easily detected and controlled by careful monitoring), to monotherapy with anti-CD20 monoclonal antibody rituximab, or more intensive chemo-immunotherapy for patients with high tumor burden (“bulky” or advanced Ann Harbor stage III and IV disease). A good response to treatment is observed in most cases, but relapses frequently occur, requiring a more intensive second-line approach, if allowed by the patient condition. As illustrated by our first case, antibody monotherapy remains an alternative in patients having some criteria of extensive disease but contraindications for a more intensive chemo-immunotherapy [16].
FL grade 3B is considered as an aggressive lymphoma and, in most cases, treated accordingly. The standard treatment combines rituximab with cyclophosphamide, doxorubicin, vincristine and prednisone [17]. However, considering a very indolent and localized case (and presumed complete surgical resection) as presented in case 2, adjuvant monotherapy may be proposed as first line approach. Careful multidisciplinary monitoring for early detection of relapse shall follow it. No progression was observed after more than 30 months of follow-up.
Conclusions
These two clinical cases emphasize the importance of an early diagnosis regarding any persistent oral lesion. A painless lymphadenopathy, an asymptomatic swelling, an ulcerated or non-ulcerated mucosal lesion or a sub-prosthetic lesion should draw attention of any oral health specialist. Lymphomas are not so rare in the oral cavity and we must not forget that local lesions can be caused by general pathology. A delayed diagnosis is detrimental for the patient when it reaches several months, while follicular lymphoma prognosis is very good with early diagnosis and appropriate therapy [2-18].
Acknowledgments
The authors kindly thank Dr Bruno Lioure (Department of Hematology) and Dr Fabrice Hubele (Nuclear Medicine Imaging Unit) for their helpful contribution.
Conflict of Interest
The authors do not declare any conflict of interest.
| References | ▴Top |
- DePena CA, Van Tassel P, Lee YY. Lymphoma of the head and neck. Radiol Clin North Am. 1990;28(4):723-743.
pubmed - Scherfler S, Freier K, Seeberger R, Bacon C, Hoffmann J, Thiele OC. Cranio-maxillofacial non-Hodgkin's lymphoma: clinical and histological presentation. J Craniomaxillofac Surg. 2012;40(7):e211-213.
doi pubmed - van der Waal RI, Huijgens PC, van der Valk P, van der Waal I. Characteristics of 40 primary extranodal non-Hodgkin lymphomas of the oral cavity in perspective of the new WHO classification and the International Prognostic Index. Int J Oral Maxillofac Surg. 2005;34(4):391-395.
doi pubmed - Silva TD, Ferreira CB, Leite GB, de Menezes Pontes JR, Antunes HS. Oral manifestations of lymphoma: a systematic review. Ecancermedicalscience. 2016;10:665.
doi pubmed - Triantafillidou K, Dimitrakopoulos J, Iordanidis F, Gkagkalis A. Extranodal non-hodgkin lymphomas of the oral cavity and maxillofacial region: a clinical study of 58 cases and review of the literature. J Oral Maxillofac Surg. 2012;70(12):2776-2785.
doi pubmed - Sebban C, Chassagne-Clement C, Nicolas-Virelizier E, Ghesquieres H. Lymphomes folliculaires. EMC-Hematologie. 2014;9:1‑18.
- Argyris PP, Dolan M, Piperi E, Tosios KI, Pambuccian SE, Koutlas IG. Oral follicular lymphomas. A short report of 8 cases with assessment of the IGH/BCL2 gene fusion with fluorescence in situ hybridization. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116(3):343-347.
doi pubmed - Tageja N, Padheye S, Dandawate P, Al-Katib A, Mohammad RM. New targets for the treatment of follicular lymphoma. J Hematol Oncol. 2009;2:50.
doi pubmed - Jordan RC, Speight PM. Extranodal non-Hodgkin's lymphomas of the oral cavity. Curr Top Pathol. 1996;90:125-146.
doi - Ferry JA, Harris NL. Lymphomas and lymphoid hyperplasia in head and neck sites. In: Pilch BZ, editor. Head and Neck Surgical Pathology. 1st ed. Philadelphia: Lippincott Williams and Wilkins; 2001. p. 476-533.
- Kolokotronis A, Konstantinou N, Christakis I, Papadimitriou P, Matiakis A, Zaraboukas T, Antoniades D. Localized B-cell non-Hodgkin's lymphoma of oral cavity and maxillofacial region: a clinical study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99(3):303-310.
doi pubmed - Kotwaney S, Shetty P. Misleading lymphomas of the oral cavity - An institutional review. Univers Res J Dent. 2014;4:145-147.
doi - Anjomshoaa I, Bulford LA, Dym H, Woo SB. Florid follicular lymphoid hyperplasia of the hard palatal mucosa managed with intralesional steroids: a case report and review of the literature. J Oral Maxillofac Surg. 2013;71(7):1202-1208.
doi pubmed - Saund D, Kotecha S, Rout J, Dietrich T. Non-resolving periapical inflammation: a malignant deception. Int Endod J. 2010;43(1):84-90.
doi pubmed - Kemp S, Gallagher G, Kabani S, Noonan V, O'Hara C. Oral non-Hodgkin's lymphoma: review of the literature and World Health Organization classification with reference to 40 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105(2):194-201.
doi pubmed - Dreyling M, Ghielmini M, Rule S, Salles G, Vitolo U, Ladetto M, Committee EG. Newly diagnosed and relapsed follicular lymphoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2016;27(suppl 5):v83-v90.
doi pubmed - Tilly H, Gomes da Silva M, Vitolo U, Jack A, Meignan M, Lopez-Guillermo A, Walewski J, et al. Diffuse large B-cell lymphoma (DLBCL): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015;26(Suppl 5):v116-125.
doi pubmed - Ahossi V, Boisrame-Gastrin S, Perrot G, Tazi M, Larras P, Perrin D. Lymphome non hodgkinien a localisation mandibulaire: a propos de deux observations. Med Buccale Chir Buccale. 2006;12:21‑29.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


