| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Case Report
Volume 5, Number 3, September 2016, pages 106-109
Diffuse Large B-Cell Lymphoma Presenting as an Endobronchial Mass: A Case Report and Review of Literature
Nithin Thomasa, d, Remiya Roycea, Vinay Garlapatia, Vera Platskyb, Horace Tangc, Thandavababu Chelliahc
aDepartment of Medicine, Coney Island Hospital, 2601 Ocean Parkway, Brooklyn, NY 11235, USA
bDepartment of Pathology, Coney Island Hospital, 2601 Ocean Parkway, Brooklyn, NY 11235, USA
cDepartment of Hematology Oncology, Coney Island Hospital, 2601 Ocean Parkway, Brooklyn, NY 11235, USA
dCorresponding Author: Nithin Thomas, Department of Medicine, Coney Island Hospital, 2601 Ocean Parkway, Brooklyn, NY 11235, USA
Manuscript accepted for publication July 15, 2016
Short title: Diffuse Large B-Cell Lymphoma
doi: http://dx.doi.org/10.14740/jh283w
| Abstract | ▴Top |
Diffuse large B-cell lymphoma (DLBCL) is the most common histological subtype of non-Hodgkin lymphoma (NHL). DLBCL normally presents with nodal involvement in the neck or the abdomen. Extranodal extramedullary disease is seen in up to 40% of cases. However, endobronchial involvement is very rare. Here we describe a 77-year-old woman with a history of bronchial asthma presenting with cough and shortness of breath who was initially treated for exacerbation of asthma. Persistent symptoms lead to further evaluation including CT scan and bronchoscopy, resulting in the diagnosis of DLBCL in this woman presenting as an endobronchial lesion. This case demonstrates the importance of considering lymphoma as a differential diagnosis of an isolated endobronchial lesion.
Keywords: Diffuse large B-cell lymphoma; Non-Hodgkin lymphoma; Endobronchial mass
| Introduction | ▴Top |
Diffuse large B-cell lymphoma (DLBCL) is the most common histological subtype of non-Hodgkin lymphoma (NHL) [1]. Patients present with rapidly enlarging lymph nodal mass in the neck or abdomen or as a mediastinal mass in primary mediastinal lymphoma. Systemic B symptoms such as fever, weight loss, and night sweats are observed in approximately 30% of patients. Bone marrow involvement is seen in up to 30% of cases [2] and extranodal extramedullary disease in up to 40% of the cases [3]. The most common site of DLBCL’s extranodal involvement is the stomach and the gastrointestinal tract, but the disease can virtually affect any tissue. However, primary pulmonary NHL (PPL) is uncommon, comprising < 1% of all NHL cases (3.6% of extranodal lymphomas and 0.5-1% of primary pulmonary malignancies) [4-6]. Endobronchial Hodgkin disease is not uncommon but is very rare in NHL, even in advanced disease [7]. Only a few cases have been reported in the literature.
| Case Report | ▴Top |
A 77-year-old woman was seen in the medical clinic for productive cough and shortness of breath especially on exertion. She did not have fever or night sweats. The patient had a history of bronchial asthma, hypertension and osteoarthritis. Her hypertension was well controlled on medications chlorthalidone, angiotensin receptor blocker and beta blocker. She was also on aspirin 81 mg daily. She had never smoked. She had no allergies. She was treated for exacerbation of asthma with inhaled albuterol, inhaled and oral steroids and oral antibiotics. Over the next 2 weeks, her symptoms had improved but did not resolve. The cough and dyspnea increased when the steroids were tapered and discontinued. At this time, the patient’s effort tolerance was reduced to walking less than a block due to shortness of breath. The patient was admitted to the hospital for evaluation.
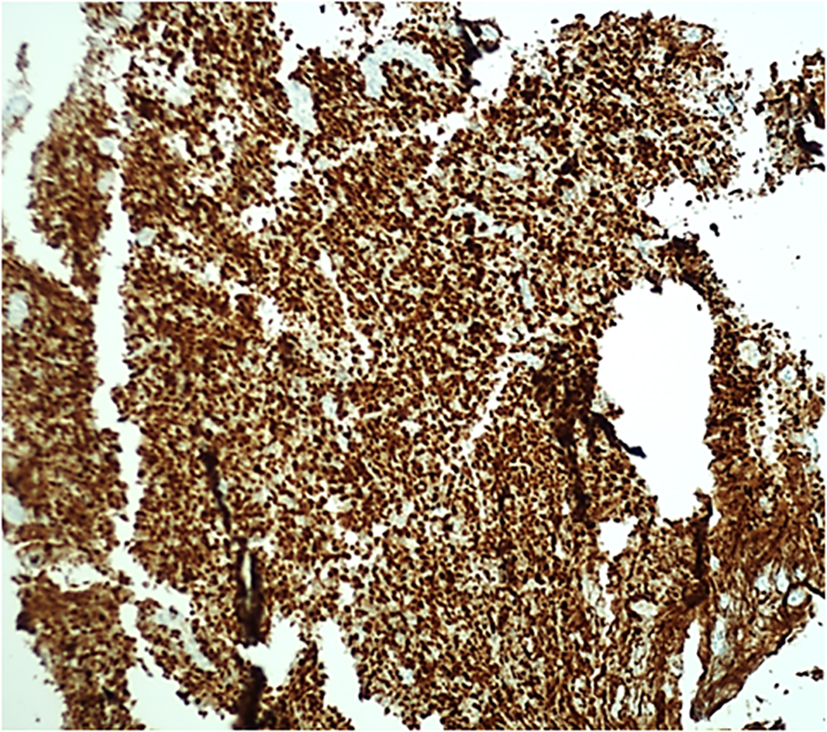
On exam, her respiration was 22/min, heart rate was 66/min, blood pressure was 122/72 mm Hg, temperature was 98.6 °F and oxygen saturation was 96% on room air. There was no pallor of the conjunctiva and no palpable lymph nodes. On auscultation of the lung, normal breath sounds were heard on both sides with wheeze over the left inframammary and infrascapular areas. Heart sounds were normal. Palpation of the abdomen showed no hepatosplenomegaly. Results of complete blood count, comprehensive chemistry, probrain natriuretic peptide and lactate dehydrogenase were all normal. A chest X-ray showed minimal left basal atelectasis. Echocardiogram showed normal left ventricular ejection fraction of 55%. CT scan of the chest with IV contrast was done and revealed a 3.7 × 2.5 cm left hilar mass extending into the proximal left main bronchus (Fig. 1). No other lesions were noted in the lung. Patient underwent bronchoscopy which showed an endobronchial lesion in the left main bronchus 2 cm away from the carina (Fig. 2). Biopsy of the mass showed bronchial tissue replaced by atypical lymphoid infiltrate of medium to large cells. Focal area of necrosis was noted, and few clusters of epithelial cells were also noted. Mitotic figures were present (Fig. 3). Immunostaining was positive for CD20 (Fig. 4) and MUM1 (Fig. 5) and negative for bcl 6 and bcL-2. Ki67 was 50%. A diagnosis of DLBCL, activated B-cell type (ABC), was made. A PET-CT scan showed hypermetabolic left hilar mass with no abnormal uptake in any other area including the bone marrow (Fig. 6). The patient was staged as primary pulmonary DLBCL stage IE. The patient was started on rituximab-CHOP chemotherapy with complete resolution of her symptoms after the first cycle.
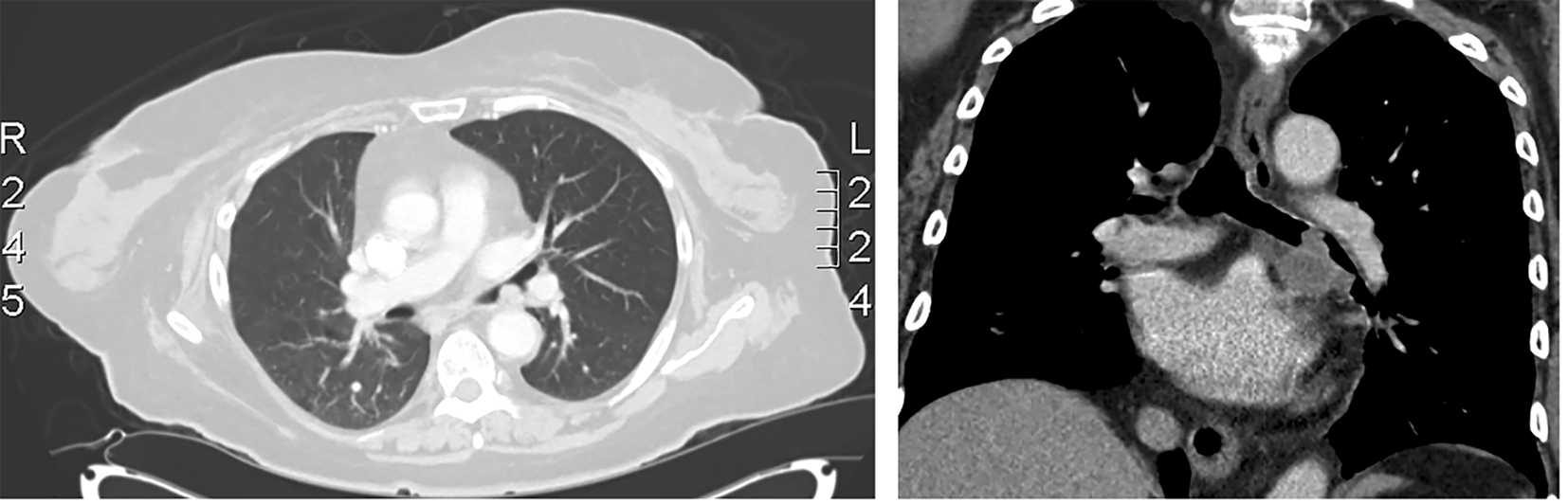 Click for large image | Figure 1. CT chest showing left endobronchial mass. |
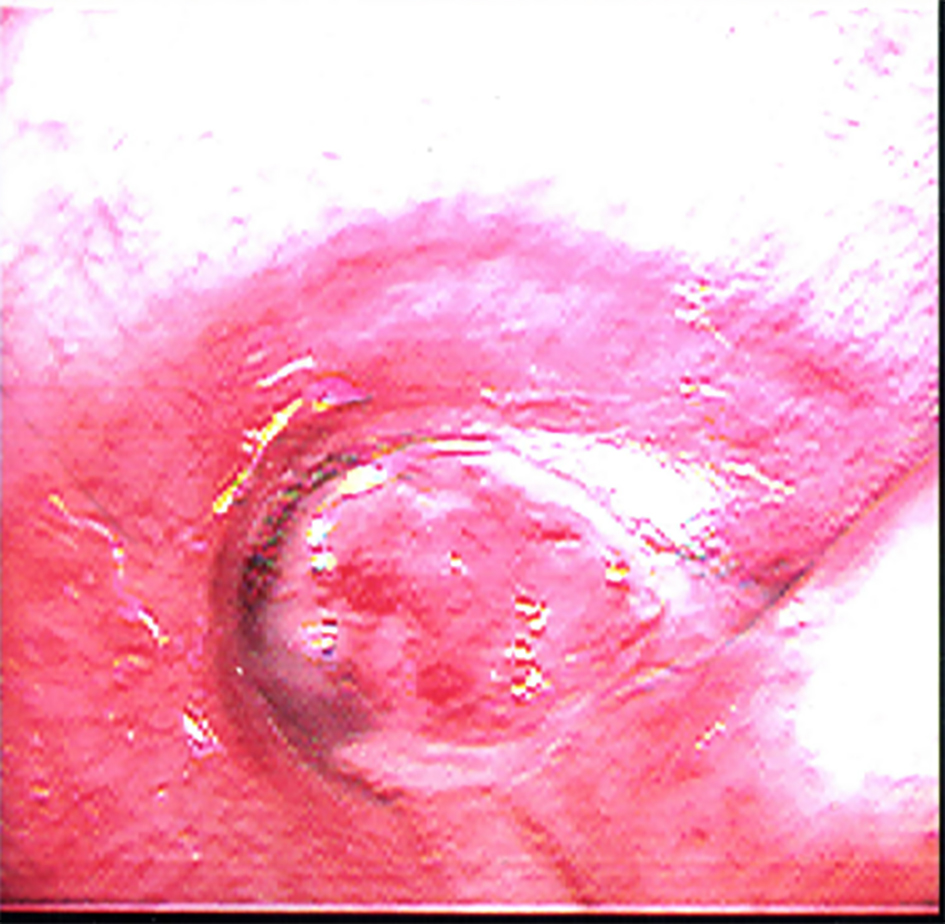 Click for large image | Figure 2. Bronchoscopic image of left mainstem bronchus showing endobronchial mass. |
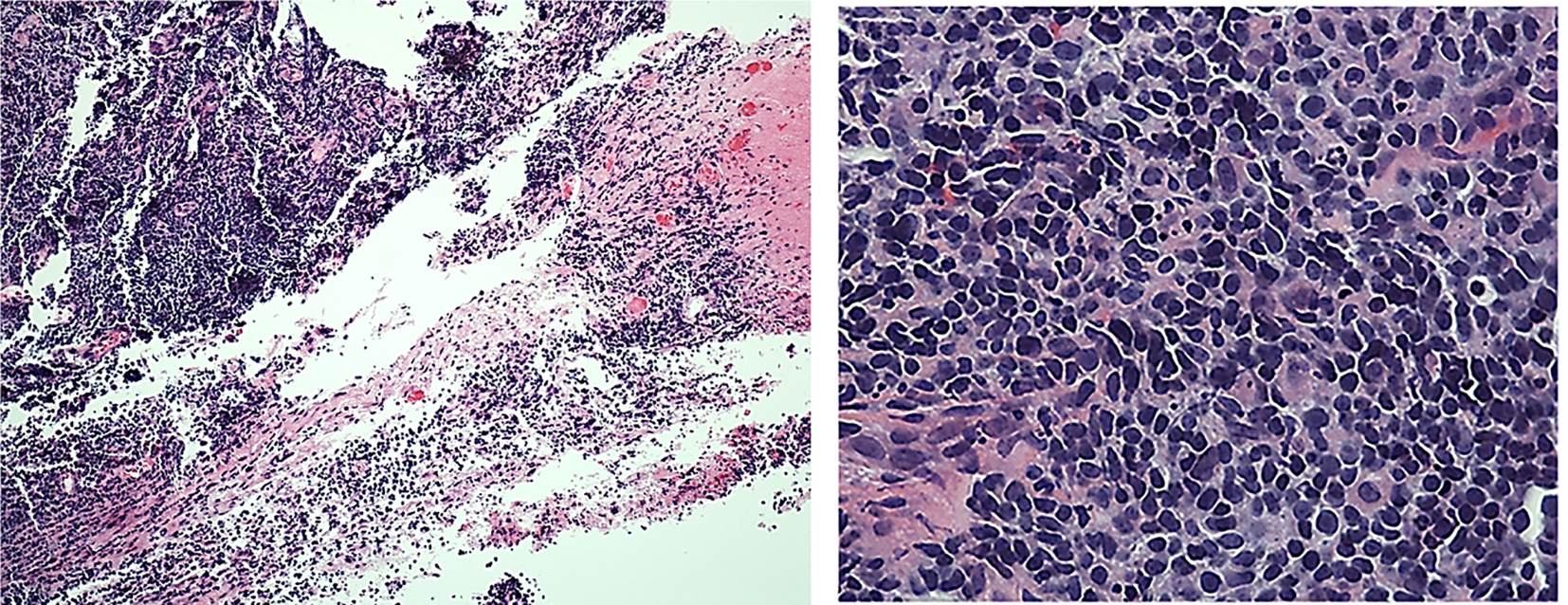 Click for large image | Figure 3. Histopathology of endobronchial lesion showing bronchial tissue being replaced by atypical lymphoid infiltrate. |
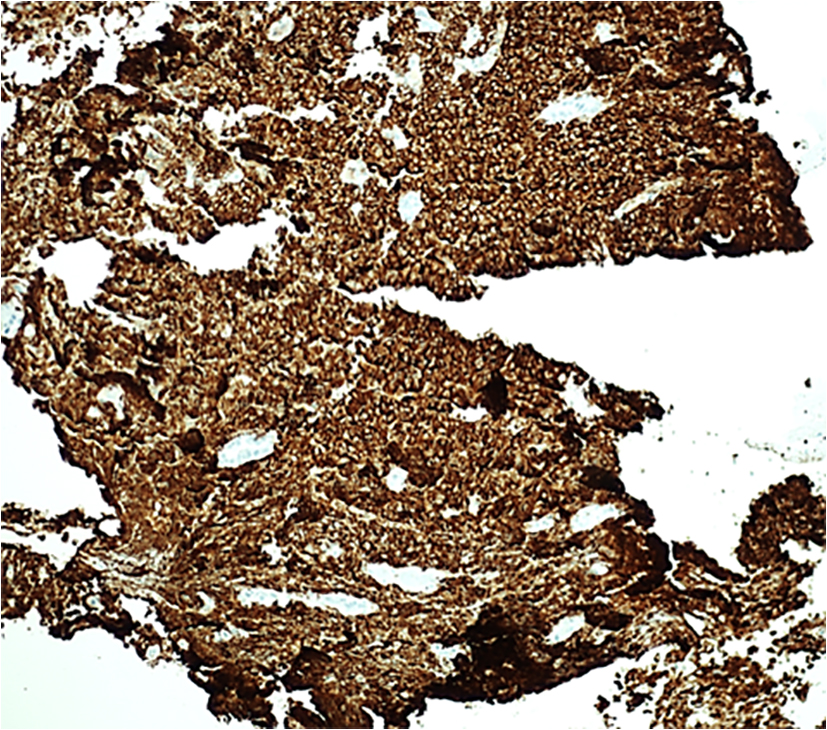 Click for large image | Figure 4. Immunostaining showing positive CD20. |
 Click for large image | Figure 5. Immunostaining showing positive MUM1. |
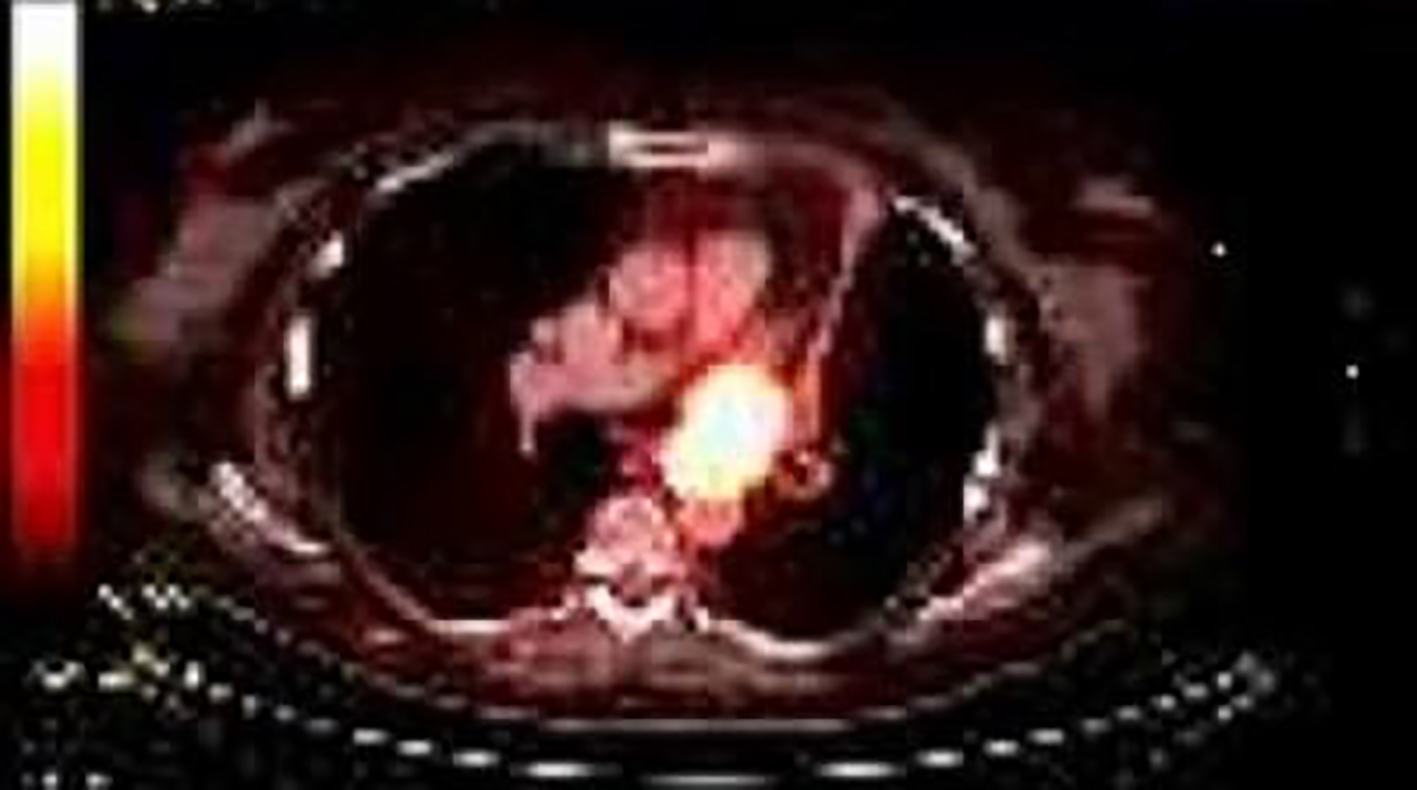 Click for large image | Figure 6. PET scan showing hypermetabolic left hilar mass. |
| Discussion | ▴Top |
PPL is uncommon. Inclusion criteria for PPL vary based on authors. Some authors include only isolated pulmonary parenchymal disease, while others consider hilar or mediastinal involvement in the absence of extrathoracic involvement [8]. Saltzstein considered lymphoma to be primary pulmonary if it affected the lungs, with or without involvement of hilar or mediastinal lymph nodes, with no other evidence of extrathoracic disease for at least 3 months after initial diagnosis [9]. Our patient satisfies the above criteria. Endobronchial lymphoma refers mainly to either secondary invasion of bronchi from adjacent nodes or discrete nodules arising within the bronchi [10].
Patients with PPL usually present with either localized respiratory symptoms due to endobronchial growth or systemic symptoms related to lymphoma. In a review of eight cases, the major presenting symptoms were dyspnea, chest pain, cough and hoarseness. The lesions are most frequently seen in the main bronchi followed by the lobar bronchi and trachea [11]. Imaging can show presence of lung collapse in approximately half of cases with a mass or hilar shadow is noted in 20% [7]. Our patient’s CT showed left hilar mass extending into left main stem bronchus.
Two patterns of disease have been described for endobronchial lymphoma. Type I is characterized by presence of diffuse submucosal nodules in the airways in individuals with systemic lymphoma. This is associated with significant pulmonary parenchymal involvement. Type II consists of localized disease in the bronchus which may be due to extension from adjacent lymph nodes or arising as de novo from bronchus associated lymphoid tissue (BALT) [7]. These patients often present with symptoms and signs of airway obstruction as our patient did.
The most common histological subtype of PPL is the indolent lymphoma of the mucosa-associated lymphoid tissue type. Large B-cell lymphoma histology like our patient’s is less common (about 25% of PPL). Patients with BALT lymphoma have a better prognosis than the aggressive type of PPLs. The common diagnosis of endobronchial lesion is lung cancer. Therefore, many older patients may refuse invasive procedures like bronchoscopy for diagnosis of endobronchial lesions and opt for palliative care. However, in establishing the diagnosis, bronchoscopic biopsy must be pursued as the lesion may be a lymphoma as in our patient’s case. The outcomes are significantly better for pulmonary lymphoma than carcinoma. In conclusion, this case report demonstrates the importance of keeping lymphoid malignancies in the differential diagnosis of endobronchial mass.
| References | ▴Top |
- Morton LM, Wang SS, Devesa SS, Hartge P, Weisenburger DD, Linet MS. Lymphoma incidence patterns by WHO subtype in the United States, 1992-2001. Blood. 2006;107(1):265-276.
doi pubmed - Sehn LH, Scott DW, Chhanabhai M, Berry B, Ruskova A, Berkahn L, Connors JM, et al. Impact of concordant and discordant bone marrow involvement on outcome in diffuse large B-cell lymphoma treated with R-CHOP. J Clin Oncol. 2011;29(11):1452-1457.
doi pubmed - Moller MB, Pedersen NT, Christensen BE. Diffuse large B-cell lymphoma: clinical implications of extranodal versus nodal presentation - a population-based study of 1575 cases. Br J Haematol. 2004;124(2):151-159.
doi pubmed - Berkman N, Breuer R, Kramer MR, Polliack A. Pulmonary involvement in lymphoma. Leuk Lymphoma. 1996;20(3-4):229-237.
doi pubmed - Cadranel J, Wislez M, Antoine M. Primary pulmonary lymphoma. Eur Respir J. 2002;20(3):750-762.
doi pubmed - Ferraro P, Trastek VF, Adlakha H, Deschamps C, Allen MS, Pairolero PC. Primary non-Hodgkin's lymphoma of the lung. Ann Thorac Surg. 2000;69(4):993-997.
doi - McRae WM, Wong CS, Jeffery GM. Endobronchial non-Hodgkin's lymphoma. Respir Med. 1998;92(7):975-977.
doi - Solomonov A, Zuckerman T, Goralnik L, Ben-Arieh Y, Rowe JM, Yigla M. Non-Hodgkin's lymphoma presenting as an endobronchial tumor: report of eight cases and literature review. Am J Hematol. 2008;83(5):416-419.
doi pubmed - Saltzstein SL. Pulmonary Malignant Lymphomas and Pseudolymphomas: Classification, Therapy, and Prognosis. Cancer. 1963;16:928-955.
doi - Gollub MJ, Castellino RA. Diffuse endobronchial non-Hodgkin's lymphoma: CT demonstration. AJR Am J Roentgenol. 1995;164(5):1093-1094.
doi pubmed - Mohapatra PR, Bhuniya S, Garg S, Dimri K, Janmeja AK. Endobronchial non-Hodgkin's lymphoma presenting as mass lesion. Indian J Chest Dis Allied Sci. 2009;51(2):107-109.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


