| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Case Report
Volume 7, Number 3, September 2018, pages 116-119
A Great Mimicker in Thoracic Spine: Spinal Double Expressor Lymphoma
Muhammad Muftia, d, Khalid Nawabb, Rabia Mohammadc
aDepartment of Medicine, St. Mary Medical Center, Long Beach, CA, USA
bDepartment of Medicine, Geisinger Holy Spirit Hospital, Camp Hill, PA, USA
cDepartment of Medicine, Coney Island Hospital, Brooklyn, NY, USA
dCorresponding Author: Muhammad Mufti, St. Mary Medical Center, GME, 1050 Linden Ave, Long Beach, CA 90813, USA
Manuscript submitted April 1, 2018, accepted May 18, 2018
Short title: Spinal Lymphoma Mimicking Epidural Hematoma
doi: https://doi.org/10.14740/jh406w
| Abstract | ▴Top |
Diffuse large B-cell lymphoma (DLBCL) is one of the most common causes of non-Hodgkin’s lymphoma (NHL). Some of these DLBCLs can have genetic mutations as well as protein overexpression. The genes involved are MYC, BCL-2 and BCL-6. These are very aggressive and do not respond well to standard chemotherapy regiment. Lymphomas usually show classic signs and symptoms but rarely can present with little or no symptoms or even mimic other disease processes. Here we will present a case where a spinal lymphoma mimicked a hematoma and the patient developed signs and symptoms only after mechanical fall and hitting his back.
Keywords: Diffuse large B-cell lymphoma; Double hit lymphoma; Double expressor lymphoma; Non-Hodgkin’s lymphoma; NHL; DHL; DEL; DLBCL
| Introduction | ▴Top |
Diffuse large B-cell lymphoma (DLBCL) is one of the most common causes of non-Hodgkin’s lymphoma (NHL). Some of these DLBCLs can have genetic mutations as well as protein overexpression. The genes involved are MYC, BCL-2 and BCL-6. Protein overexpression can be seen on immunohistochemistry (IHC) and genetic mutations in the florescent in situ hybridization (FISH) analysis. DLBCL with just two protein overexpressions are classified as double expressor lymphomas (DELs), while the ones with two chromosomal mutations are called double hit lymphomas. If all three genes are involved, it will be triple expressor/triple hit lymphoma respectively.
| Case Report | ▴Top |
A 39-year-old male with a history of human immunodeficiency virus (HIV) and multiple psychiatric issues initially presented to the emergency room (ER) after falling while cycling, landing on his back and complaining of pain in the lower back. A bony injury was ruled out with spinal X-ray and patient was ambulating with no neurological symptoms; therefore, he was discharged to home.
The patient presented to the ER again after 2 weeks, reporting that the back pain had persisted, and he had developed tingling, numbness and weakness in his lower extremities, requiring him to use a cane for ambulation. Also reported difficulty urinating that started the night before. Patient’s physical exam was inconsistent, with being able to move his lower extremities without a problem at times, and at others, barely moving his legs, mostly complaining of pain. A stat MRI of the spine was done. Lumbar MRI was unremarkable, but thoracic MRI revealed a large right posterior epidural mass extending from T3 to T7, 10.9 cm craniocaudally by 1.6 cm transverse by 1.6 cm anteroposteriorly, causing severe compression of the spinal cord, displacing it to the left anteriorly (Figs. 1 and 2). The mass was extending to the right T4-T8 neural foramina. It was isointense on T1- and T2-weighted imaging. Considering the patient’s history of recent trauma, the mass was read as an epidural hematoma by the radiologist. Neurosurgery was consulted, and they decided to take the patient to the operating room for evacuation of the presumed hematoma.
 Click for large image | Figure 1. MRI spine lateral view showing the mass in the thoracic spine. |
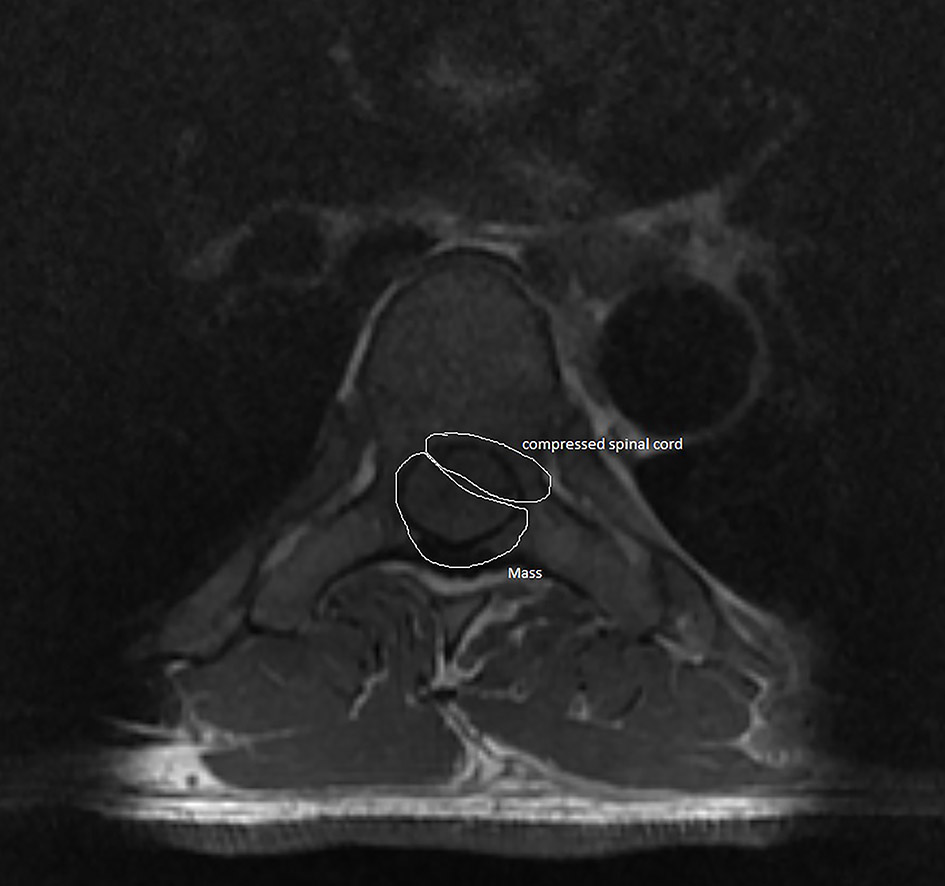 Click for large image | Figure 2. MRI spine axial view showing the mass compressing the spinal cord. |
When the epidural space was opened, no hematoma was visualized. Instead, a soft tissue epidural mass was seen, which was removed in a piecemeal fashion, and specimen was sent for histopathology. Postoperatively, the patient reported some improvement in his weakness and numbness in lower extremities, with the resolution of the tingling. Immunohistopathology of the specimen revealed Epstein-Barr virus (EBV)-positive high-grade B-cell lymphoma overexpression BCL-2 and C-MYC on IHC. FISH studies were sent were indicative of MYC gene rearrangement and trisomy 14, IgH gene duplication/rearrangement with a chromosome other than chromosome 18. The patient was diagnosed with DEL. The patient was started on dose-adjusted EPOCH-R regiment, and an Omaya reservoir was placed. The patient was discharged to a skilled nursing facility once he was stable to follow up outpatient with the oncologist.
| Discussion | ▴Top |
DLBCL is one of the most causes of NHL. It occurs in about 25% of NHL cases [1]. The prognosis of lymphoma is estimated using tools such as international prognostic index. DLBCL is classified into many diagnostic subtypes per WHO 2016 classification. WHO classification also stratifies certain overlap categories which include high-grade B-cell lymphoma and unclassifiable B-cell lymphoma.
DLBCL occurs in about seven per 100,000 people per year [1]. The incidence varies based on the race being the highest in Caucasians followed by Black, Asian. American Indian or Alaska natives. The median age of presentation is 64 years, but there have been cases of younger people presenting with the disease [2]. Development of NHL is considered AIDS-defining characteristic in a patient infected with HIV, and it occurs in about 10% of HIV-positive patients [3]. HIV patients are also predisposed to more primary central nervous system NHL than people without the disease.
Spinal lymphomas are rare and only comprise about 1-2% of all lymphomas and about 10% of the epidural tumors [4]. These tumors can remain indolent for years at a time while other times it can be highly aggressive. Spinal lymphomas are not well defined and usually seen rarely. These tumors when found in sites other than the spine can present with symptoms such as fever, night sweats and weight loss (B-type symptoms) with enlarged lymph nodes. On the other hand, when the spine is involved, the symptoms can be of cord compression, cauda equina or paresthesia. Cho et al presented a patient who had numbness and tingling at time of presentation [5], and Mally et al described the patient with low back pain radiating to the left lower limb, tingling numbness and weakness of 6-month duration [6]. Lyons et al retrospectively studied eight patients presenting with symptoms of paresthesias, hyperreflexia and paraplegia all found to have primary spinal epidural NHL. The median age for patients in this report was 70 years [7].
Double hit lymphoma is a subtype where there is overexpression of genes which are involved in apoptosis or proliferation. The genes involved in apoptosis in lymphoma are BCL-2 and BCL-6. MYC overexpression results in uncontrolled proliferation of the cells. The translocations associated with these genes can be t(14;18) and t(8;14) or t(8;22). Translocation of (14;18) usually observed in Burkitt lymphoma is seen in about 85% Europeans and 70% Asians [4], but in DLBCL it is seen anywhere between 5% and 30% of the cases [8]. MYC overexpression happens with translocation of (8;22) in about 14% of cases of DLBCL [9]. Three gene overexpression can occur in about 8% of the cases called triple hit lymphoma [9]. These will include MYC, BCL-2 and BCL-6. Other rare genes described in the literature include CCND1, BCL3 and PAX5 [10]. For detection of these gene translocations, FISH or IHC can be used. FISH is the gold standard [11] but an expensive test; on the other hand, IHC is much cheaper but not as sensitive or specific and depends on the cutoff value used by the laboratory.
Some lymphomas can have overexpression of the proteins MYC and BCL-2 or BCL-6 seen on IHC but do not have the genetic mutation detected in the FISH analysis. These are known as DEL or triple expressor lymphoma if all three are seen. Hu et al showed that patients with DEL had worse outcomes than DLBCL without it [12].
Different treatment modalities have been tried for treating DHL and DEL. At the time of writing this case report, there is no standard of care guideline for treating it. The modalities available include dose-adjusted EPOCH-R (etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, rituximab), RHyper-CVAD (cyclophosphamide, vincristine, doxorubicin and dexamethasone alternating with high-dose methotrexate and cytarabine and use of rituximab), R-CODOX-M/R-IVAC (rituximab-cyclophosphamide, vincristine, doxorubicin with methotrexate/ifosfamide, etoposide and cytarabine) and R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, prednisone). The R-CHOP therapy has fallen out of favor as it has inferior outcomes compared to the intensive regiments mentioned above. Autologous stem cell transplants are not part of the current guidelines, but they have been used in various trials as consolidative therapy with mixed results. Other approaches are also being tried which includes using body’s own T cells to fight against the malignancy. The modified T-cell therapy called chimeric antigen receptor T cells is also approved by FDA for patients with relapsed progressing lymphoma with two prior treatments failures.
Wilson et al showed that dose-adjusted EPOCH-R had good efficacy for treatment of DLBCL and rituximab helped overcome the adverse effects of BCL-2 and BCL-6 [13]. Another study was done by Landsburg et al which focused on outcomes of DHL patients who attained complete remission after first-line therapy and were deemed fit for autologous stem cell transplant (ASCT) [14]. These patients were followed for overall survival (OS) and relapse-free survival (RFS). The study showed that OS and RFS were about 80% and 87% for all patient groups and there was no difference in survival in ASCT group versus non-ASCT group. Kawashima et al retrospectively looked at OS and progression-free survival (PFS) of patients with DEL who underwent an allogeneic transplant. They found that both OS and PFS were lower in patients with DEL than those without DEL [15]. Herrera et al analyzed patients with relapsed DHL or DEL undergoing ASCT and found that they had inferior outcomes [16].
Newer targeted agents are being developed and tested for the treatment of aggressive lymphomas. Some of the current ongoing clinical trials include use of ibrutinib to control lymphoma after ASCT in DHL patients (terminated for slow accrual) [ClinicalTrials.gov Identifier: NCT02272686], monoclonal antibody against PD-L1, currently in phase II trial, durvalumab after ASCT [ClinicalTrials.gov Identifier: NCT03241017] and finally the use of novel agent Venetoclax (selective BCL-2 inhibitor) with dose-adjusted EPOCH-R for treatment of aggressive B-cell lymphomas [ClinicalTrials.gov Identifier: NCT03036904]. MYC inhibitor agents being investigated include BET bromodomain inhibitors which had a remarkable response in phase I clinical trials which work by inhibiting MYC-driven transcriptional factors [17] [ClinicalTrials.gov Identifier: NCT01943851 and NCT01949883]. Some other agents developed earlier failed to show significant clinical response, the so-called Aurora kinase A and B inhibitors [18]. The CAR T-cell therapy has shown that promising results in relapsed or refractory DLBCL [19] were recently approved by FDA. For DEL there is currently an ongoing phase III clinical trial to combine the use of thalidomide with R-CHOP regiment [ClinicalTrials.gov identifier: NCT03318835].
Our patient presented after a trauma to the back, and initial imaging was negative for any acute fractures. Soon afterward he started developing paresthesia and ascending weakness which prompted the physician to perform MRI of the back which revealed T1-T2 isointense mass which was demonstrating enhancement and it was causing severe compression of the spinal cord. The patient had no B type symptoms, and the radiologist interpretation of the imaging was hematoma after trauma. Upon surgery to evacuate the hematoma the neurosurgeons realized that it was, in fact, a mass which later turned out to be an EBV-positive DEL with overexpression of MYC and BCL-2.
Conclusions
DHL and DEL are a subset of DLBCL which can be very aggressive, and rarely it can present with little to no symptoms. Suspicion should be high in a patient with known HIV status. The gene mutations lead to its aggressive behavior. Currently, there is no standard of care, but intensive regiments are favored over R-CHOP. The newer targeted agents might improve the outcomes in the future.
Acknowledgments
The authors would like to thank Dr. Omkar Marathe (Hematologist/Oncologist, St. Mary Medical Center, Long Beach, CA, USA) for reviewing the case report before submission.
| References | ▴Top |
- Morton LM, Wang SS, Devesa SS, Hartge P, Weisenburger DD, Linet MS. Lymphoma incidence patterns by WHO subtype in the United States, 1992-2001. Blood. 2006;107(1):265-276.
doi pubmed - Nicolae A, Pittaluga S, Abdullah S, Steinberg SM, Pham TA, Davies-Hill T, Xi L, et al. EBV-positive large B-cell lymphomas in young patients: a nodal lymphoma with evidence for a tolerogenic immune environment. Blood. 2015;126(7):863-872.
doi pubmed - Tossing G. Immunodeficiency and its relation to lymphoid and other malignancies. Ann Hematol. 1996;73(4):163-167.
doi pubmed - Biagi JJ, Seymour JF. Insights into the molecular pathogenesis of follicular lymphoma arising from analysis of geographic variation. Blood. 2002;99(12):4265-4275.
doi - Cho HJ, Lee JB, Hur JW, Jin SW, Cho TH, Park JY. A rare case of malignant lymphoma occurred at spinal epidural space: a case report. Korean J Spine. 2015;12(3):177-180.
doi pubmed - Mally R, Sharma M, Khan S, Velho V. Primary lumbo-sacral spinal epidural non-Hodgkin's lymphoma: a case report and review of literature. Asian Spine J. 2011;5(3):192-195.
doi pubmed - Lyons MK, O'Neill BP, Marsh WR, Kurtin PJ. Primary spinal epidural non-Hodgkin's lymphoma: report of eight patients and review of the literature. Neurosurgery. 1992;30(5):675-680.
doi - Barrans SL, Evans PA, O'Connor SJ, Kendall SJ, Owen RG, Haynes AP, Morgan GJ, et al. The t(14;18) is associated with germinal center-derived diffuse large B-cell lymphoma and is a strong predictor of outcome. Clin Cancer Res. 2003;9(6):2133-2139.
pubmed - Petrich AM, Gandhi M, Jovanovic B, Castillo JJ, Rajguru S, Yang DT, Shah KA, et al. Impact of induction regimen and stem cell transplantation on outcomes in double-hit lymphoma: a multicenter retrospective analysis. Blood. 2014;124(15):2354-2361.
doi pubmed - Cheah CY, Oki Y, Westin JR, Turturro F. A clinician's guide to double hit lymphomas. Br J Haematol. 2015;168(6):784-795.
doi pubmed - Niitsu N, Okamoto M, Miura I, Hirano M. Clinical features and prognosis of de novo diffuse large B-cell lymphoma with t(14;18) and 8q24/c-MYC translocations. Leukemia. 2009;23(4):777-783.
doi pubmed - Hu S, Xu-Monette ZY, Tzankov A, Green T, Wu L, Balasubramanyam A, Liu WM, et al. MYC/BCL2 protein coexpression contributes to the inferior survival of activated B-cell subtype of diffuse large B-cell lymphoma and demonstrates high-risk gene expression signatures: a report from The International DLBCL Rituximab-CHOP Consortium Program. Blood. 2013;121(20):4021-4031; quiz 4250.
doi pubmed - Wilson WH, Dunleavy K, Pittaluga S, Hegde U, Grant N, Steinberg SM, Raffeld M, et al. Phase II study of dose-adjusted EPOCH and rituximab in untreated diffuse large B-cell lymphoma with analysis of germinal center and post-germinal center biomarkers. J Clin Oncol. 2008;26(16):2717-2724.
doi pubmed - Landsburg DJ, Falkiewicz MK, Maly J, Blum KA, Howlett C, Feldman T, Mato AR, et al. Outcomes of patients with double-hit lymphoma who achieve first complete remission. J Clin Oncol. 2017;35(20):2260-2267.
doi pubmed - Kawashima I, Inamoto Y, Maeshima AM, Nomoto J, Tajima K, Honda T, Shichijo T, et al. Double-expressor lymphoma is associated with poor outcomes after allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2018;24(2):294-300.
doi pubmed - Herrera AF, Mei M, Low L, Kim HT, Griffin GK, Song JY, Merryman RW, et al. Relapsed or refractory double-expressor and double-hit lymphomas have inferior progression-free survival after autologous stem-cell transplantation. J Clin Oncol. 2017;35(1):24-31.
doi pubmed - Xu Y, Vakoc CR. Targeting cancer cells with BET bromodomain inhibitors. Cold Spring Harb Perspect Med. 2017;7(7).
doi pubmed - Friedberg JW, Mahadevan D, Cebula E, Persky D, Lossos I, Agarwal AB, Jung J, et al. Phase II study of alisertib, a selective Aurora A kinase inhibitor, in relapsed and refractory aggressive B- and T-cell non-Hodgkin lymphomas. J Clin Oncol. 2014;32(1):44-50.
doi pubmed - Kochenderfer JN, Dudley ME, Kassim SH, Somerville RP, Carpenter RO, Stetler-Stevenson M, Yang JC, et al. Chemotherapy-refractory diffuse large B-cell lymphoma and indolent B-cell malignancies can be effectively treated with autologous T cells expressing an anti-CD19 chimeric antigen receptor. J Clin Oncol. 2015;33(6):540-549.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


