| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Case Report
Volume 6, Number 4, October 2017, pages 101-104
Revisiting Howell-Jolly Body-Like Cytoplasmic Inclusions in Neutrophils: A Report of Two Cases and Confirmation of Nuclear Origin
Reeba Ommana, Christina Kwonga, Daniel Shepherda, Jo A. Molnara, Milind M. Velankara, Kamran M. Mirzaa, b
aDepartment of Pathology, Loyola University Medical Center, Maywood, IL 60153, USA
bCorresponding Author: Kamran M. Mirza, Department of Pathology, Loyola University Medical Center, EMS 2234, Bldg 210, 2160 S. First Avenue, Maywood, IL 60153, USA
Manuscript submitted June 18, 2017, accepted July 26, 2017
Short title: Cytoplasmic Inclusions in Neutrophils
doi: https://doi.org/10.14740/jh334w
| Abstract | ▴Top |
Howell-Jolly body-like inclusions in neutrophils have been reported in a handful of reports; however, their nuclear origin has never been confirmed to date. We report the presence of these cytoplasmic inclusions in two cases and confirm their DNA-based origin by fluorescent nuclear staining. Peripheral blood smears were manually reviewed by light microscopy and after 4',6-diamidino-2-phenylindole (DAPI) fluorescent staining via confocal microscopy. Methanol fixed peripheral blood smears were incubated with DAPI (Sigma Aldrich, St. Loius, MO, USA) and coverslipped with mounting media. DAPI-stained cells were imaged with a Leica SPE confocal microscope using a 405 nm excitation laser and a 63×/1.3 NA oil immersion objective. Optical sections spanning the entire cell thickness were acquired and maximum intensity projections were produced in ImageJ. Both cases described herein had Howell-Jolly body-like inclusions similar to those reported in the literature. Testing for relevant infectious etiologies was negative. Positive staining on fluorescence microscopy confirmed DNA-based origin of this cytoplasmic inclusion material. These DNA-based inclusions occur in the immunosuppressed patient and mimic infectious inclusions. While morphologically worrisome, recognition of these inclusions may prevent unnecessary treatment and testing in clinically appropriate patients.
Keywords: Cytoplasmic inclusions; Neutrophils; Howell-Jolly body-like
| Introduction | ▴Top |
From the Auer rod to the Döhle body, the identification of cytoplasmic inclusions in circulating granulocytic cells is clinically relevant and often carries prognostic implications [1]. Howell-Jolly body-like cytoplasmic inclusions in neutrophil cytoplasm, aptly named due to the morphologic similarity to their erythrocytic counterparts, have been reported in a very small number of reported cases [2-6]. The presence of these spherical, basophilic inclusions within the cytoplasm of neutrophils raises immediate concern for an infectious etiology, the main differential of which is typically either Anaplasmosis or Ehrlichiosis, which presents with similar appearing cytoplasmic inclusions [7]. To complicate matters, such inclusions have, to date, only been reported in immunosuppressed patients making an infectious etiology very likely. While this inclusion has been assumed to be nuclear in origin, this has not been proven to date [5]. Here we report two cases with these inclusions in patients on tacrolimus for post-transplant immunosuppressive therapy. Additionally, using 4',6-diamidino-2-phenylindole (DAPI) fluorescence staining, we confirm herein that this fragment is indeed comprised of nuclear material.
| Case Reports | ▴Top |
Case 1
Patient 1 was a 72-year-old male with past medical history of deep vein thrombosis, coronary artery disease status post coronary artery bypass grafting, type II diabetes mellitus, hypothyroidism, and stage IV chronic kidney disease, who was 2 years status post right-sided single lung transplant for interstitial lung disease (usual interstitial pneumonia, UIP). He was on tacrolimus and prednisone immunosuppression and G-CSF therapy for leukopenia. The patient was transferred to our tertiary care facility with complaints of fever, and malaise. A diagnostic workup was consistent with sepsis complicated by septic shock. Clinically, the most likely etiology for the patient’s sepsis was considered to be bacterial or viral pneumonia; however, pan-cultures were negative. Respiratory PCR was positive for Rhinovirus/Enterovirus (RV/EV). A hemogram demonstrated leukopenia with absolute neutropenia, an absolute lymphopenia, macrocytic anemia and thrombocytopenia. Review of the peripheral blood smear (Fig. 1) demonstrates the presence of dense basophilic cytoplasmic (Howell-Jolly body-like) inclusions in many circulating neutrophils. This finding was immediately reported to the clinical team and studies for Ehrlichia chaffeensis and Anaplasmosis phagocytophilum were sent. The patient was empirically started on doxycycline therapy. The tests were eventually reported as “within range”, indicating lack of both IgM and IgG antibodies to either pathogen. The patient was treated and discharged in stable condition 5 days later with follow-up in clinic. Subsequently, he developed weakness and was readmitted after a fall. Clinical evaluation revealed sepsis without clear cause. His hospital course was complicated by an ICU stay, intubation and eventual tracheostomy. He was eventually discharged on full ventilatory support; however, he became gradually unresponsive to stimuli and expired soon after discharge.
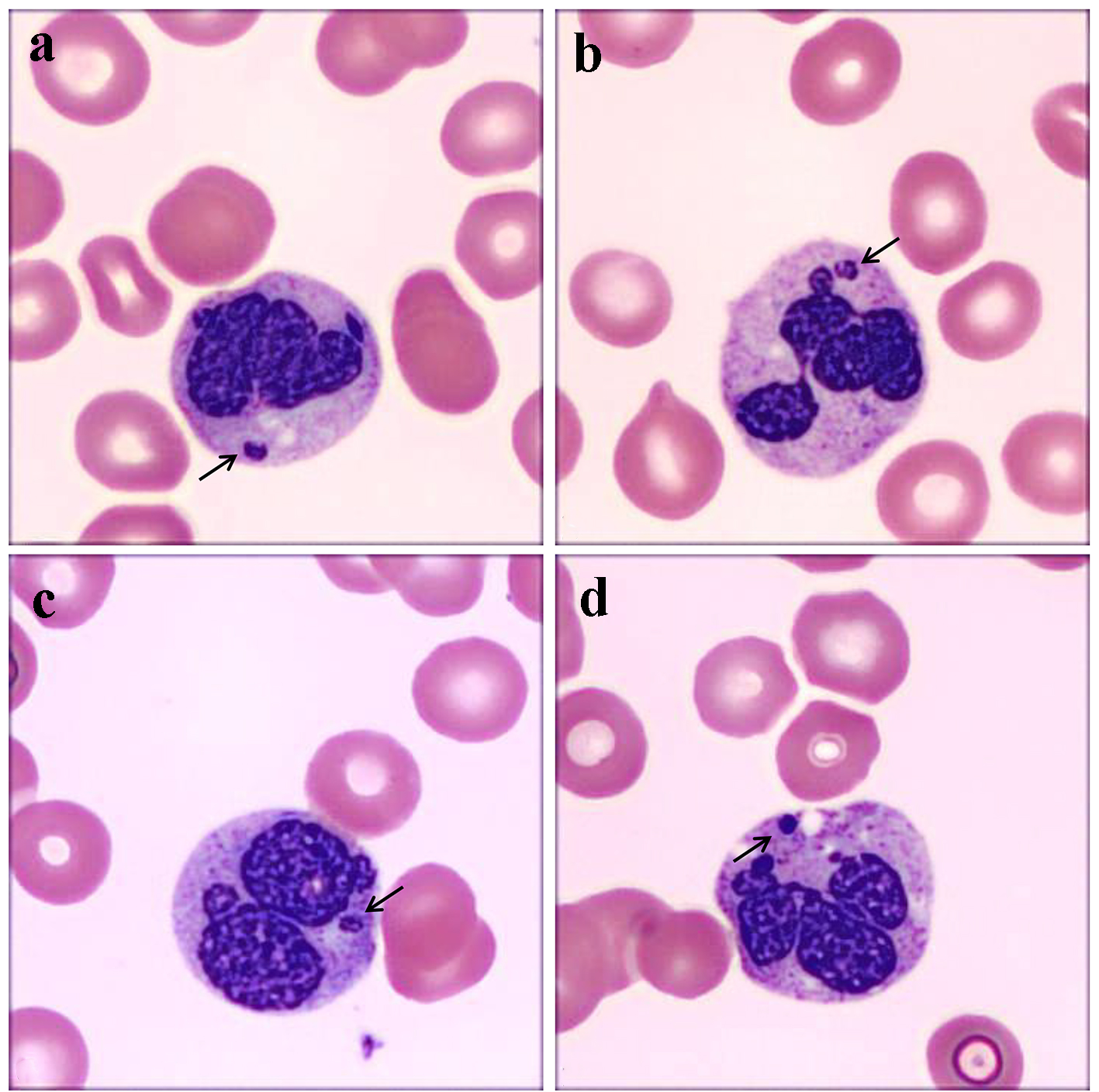 Click for large image | Figure 1. (a-d) Spherical Howell-Jolly body-like inclusions within neutrophil cytoplasm from case 1 (a and b) and 2 (c and d) highlighted by short black arrows. These inclusions are separate from the main nuclear body and demonstrate a similar basophilic staining pattern on the Wright Giemsa stain. The main nucleus demonstrates a coarsely condensed chromatin. The secondary neutrophilic granules demonstrate some toxic change, more pronounced in d. |
Case 2
Patient 2 was a 67-year-old male with past medical history of coronary artery disease status post coronary artery bypass grafting and type II diabetes mellitus who was 1 month status post liver transplant for non-alcoholic steatohepatitis (NASH)-related cirrhosis on mycophenolate mofetil and tacrolimus immunosuppression. He presented with melena, worsening anemia and fluid overload. A hemogram demonstrated normocytic anemia, lymphopenia, left shift to immaturity in circulating granulocytic cells and Howell-Jolly body-like inclusions in neutrophils (Fig. 1). Similar to case 1, this finding was immediately reported to the clinical team and testing for Ehrlichia chaffeensis and Anaplasmosis phagocytophilum was sent out while the patient was started on doxycycline prophylactically. The tests were reported as within range, indicating lack of IgM and IgG presence of the antibodies to either pathogen. The patient’s clinical course was complicated by Klebsiella bacteremia, MRSA pneumonia and respiratory failure. After several months of hospitalization, the patient was eventually stabilized and sent home. Although he did well on several follow-up appointments, the patient eventually expired 3 months after discharge.
| Discussion | ▴Top |
Named after William Howell and Justin Jolly, true Howell-Jolly bodies are nuclear remnants commonly seen in circulating red blood cells, most often in asplenia or in patients with diminished splenic function [8]. Howell-Jolly body-like inclusions have been described in the neutrophils of patients on immunosuppressive therapy, chemotherapeutic regimens, and in an AIDS patient with mycobacterial MAC infection [2-5, 9, 10]. While they are named because of their similarity to true Howell-Jolly bodies on the Wright Giemsa stain, the true nature of this cytoplasmic inclusion remains unknown [4]. In some reports, authors have tried various methodologies to identify the origin of these cytoplasmic inclusions, or alluded to the same; however, none have shown definitive evidence of what they comprise [2-4]. Theories of how these inclusions come to be include their being “apoptotic bodies” or akin to Barr bodies [3, 6]. However, true apoptotic bodies demonstrate apoptotic DNA fragmentation in the entire cell with no normal nucleus, while inclusions always occur in the setting of an adjacent, morphologically unremarkable nucleus. Similarly, the morphology of Barr bodies has been well documented as having drumstick appearance with a nodular end with a link to the main nucleus [11], while these inclusions are widely separated from the main nucleus. While these theories cannot be disproven, it remains more plausible that this finding is a result of medication effect since tacrolimus has been implicated in morphologic changes such as acquired Pelger–Huët change [12]. However, that still would not explain why it occurs in the setting of AIDS patients reported in the literature, to which end we postulate that it may have some link with high neutrophil turnover.
Whatever the mechanism that causes the occurrence of these inclusions, we set out to confirm their true nature is in fact nuclear fragments. We stained peripheral blood smears from both our cases with DAPI, a fluorescent stain that binds preferentially to the minor groove of A-T rich regions in DNA [13] and is commonly used as a nuclear stain for fluorescent images. Representative images from both our cases demonstrate isolated, spherical DAPI positive signals within the cytoplasm of neutrophils adjacent to clearly identifiable polymorphonuclear nuclei, consistent with the Howell-Jolly body-like inclusion (Fig. 2), confirming its nuclear origin.
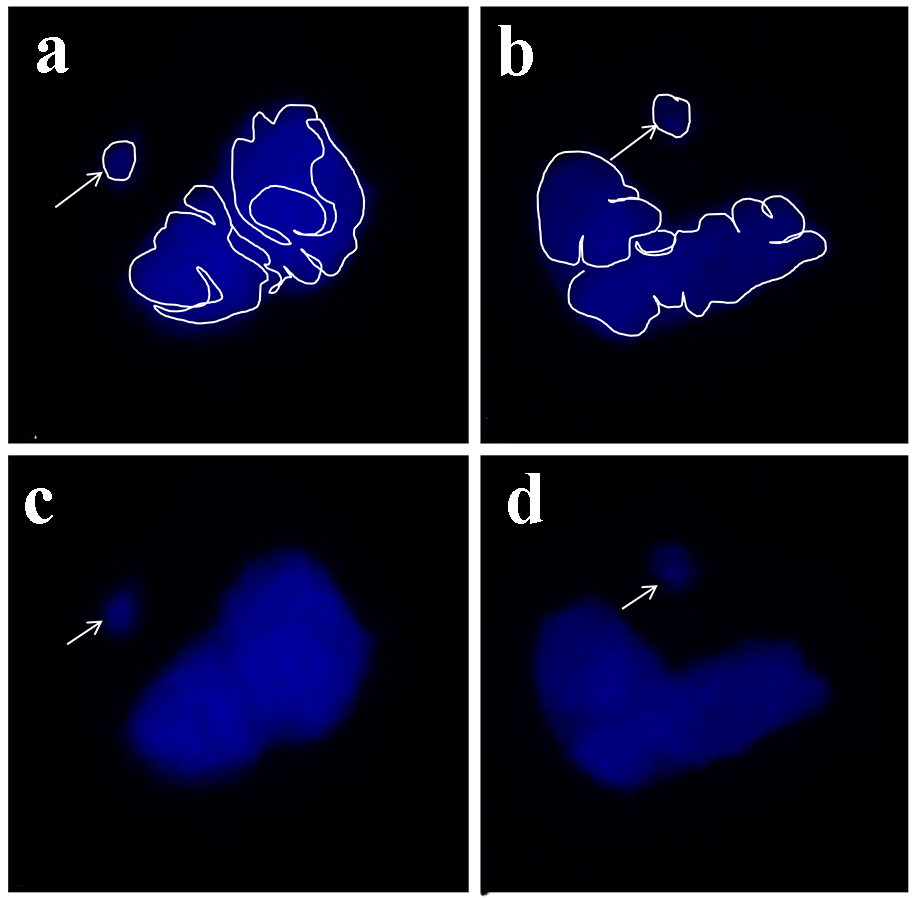 Click for large image | Figure 2. 4′,6-diamidino-2-phenylindole (DAPI) immunofluorescence microscopy images demonstrating a single distinct spherical nuclear fragment consistent with the Howell-Jolly body-like inclusion (arrows) located separate from the neutrophil nucleus in two representative nuclei in two representative neutrophils (panels a and b with nuclear features highlighted, and c and d demonstrate the same two neutrophils without highlights). |
In this report, we revisited the infrequently reported but clinically relevant cytoplasmic inclusion accurately named the Howell-Jolly body-like inclusion and confirmed its nuclear origin. Both cases reported herein had reason for immunosuppression (therapy-related), which is consistent with cases reported in the literature. While it cannot be ignored that both cases in this report succumbed to their underlying disease, no correlation can be drawn as to the presence of these inclusions with poor outcome, as too many confounding variables would need to be accounted for. Morphologically, the presence of such inclusions raises alarm for infectious causes, which should always be considered on a case-by-case basis; however, recognition of the non-infectious nature of these inclusions may prevent unnecessary treatment and testing in select patients.
| References | ▴Top |
- Seymour JF, Estey EH. The prognostic significance of auer rods in myelodysplasia. Br J Haematol. 1993;85(1):67-76.
doi - Bain BJ. Blood Cells: A Practical Guide. 1st ed. Philadelphia, PA: J. B. Lippincott; 1989.
- Slagel DD, Lager DJ, Dick FR. Howell-Jolly body-like inclusions in the neutrophils of patients with acquired immunodeficiency syndrome. Am J Clin Pathol. 1994;101(4):429-431.
doi pubmed - Kahwash E, Gewirtz AS. Howell-Jolly body-like inclusions in neutrophils. Arch Pathol Lab Med. 2003;127(10):1389-1390.
pubmed - Rowe RG, Esrick E. Howell-Jolly-like bodies in neutrophils. Blood. 2015;125(17):2729.
doi - Akhtari M, Waller EK. Howell-Jolly body-like inclusions in neutrophils. Blood. 2009;114(14):2860.
doi pubmed - Ismail N, McBride JW. Tick-borne emerging infections: ehrlichiosis and anaplasmosis. Clin Lab Med. 2017;37(2):317-340.
doi pubmed - Sears DA, Udden MM. Howell-Jolly bodies: a brief historical review. Am J Med Sci. 2012;343(5):407-409.
doi pubmed - Godwin JH, Stopeck A, Chang VT, Godwin TA. Mycobacteremia in acquired immune deficiency syndrome. Rapid diagnosis based on inclusions in the peripheral blood smear. Am J Clin Pathol. 1991;95(3):369-375.
doi pubmed - Abdel-Monem H, Prakasam A, Thiagarajan P. Howell-jolly body-like inclusions in neutrophils of a transplant recipient in association with ganciclovir therapy. Arch Pathol Lab Med. 2010;134(6):809-810.
doi pubmed - Parameshwaran N. The sex chromatin body and neutrophil 'drumstick' appendage. Ceylon Med J. 1971;16(1):39-46.
pubmed - Etzell JE, Wang E. Acquired Pelger-Huet anomaly in association with concomitant tacrolimus and mycophenolate mofetil in a liver transplant patient: a case report and review of the literature. Arch Pathol Lab Med. 2006;130(1):93-96.
pubmed - Chazotte B. Labeling nuclear DNA using DAPI. Cold Spring Harb Protoc. 2011;2011(1).
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


