| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Case Report
Volume 5, Number 3, September 2016, pages 113-115
IgG4-Related Disorder Masquerading as an Indurated Skin Lesion
Nathan Visweshwara, c, Michael Jaglalb, Stephen Malachowskia, Sana Azama, Damian Laberb, Patrick Griffinb
aUniversity of South Florida Morsani College of Medicine, Tampa, FL, USA
bMoffitt Cancer Center, Tampa, FL, USA
cCorresponding Author: Nathan Visweshwar, Department of Hematology, University of South Florida, 13330 USF Laurel Drive, Tampa, FL 33612, USA
Manuscript accepted for publication August 10, 2016
Short title: IgG4-Related Disorder
doi: http://dx.doi.org/10.14740/jh287w
| Abstract | ▴Top |
IgG4-related disorder (IgG4-RD) is a recently defined systemic disorder characterized by a unique fibro-inflammatory response that involves multiple organs including lymph nodes, salivary, lacrimal glands, and the pancreas as well as other endocrine organs. These organs display lymphoplasmacytic infiltrate with positive staining for IgG4 and high levels of circulating IgG4. We present an unusual case of IgG4-RD in a 55-year-old African-American female, who presented with an isolated chronic indurated painful mass in the thigh with a normal IgG4. Increased awareness with variable manifestations of IgG4-RD will facilitate the diagnosis of this condition.
Keywords: IgG4-related disorder; Indurated skin lesion; Immunosuppressive therapy
| Introduction | ▴Top |
IgG4-related disorder (IgG4-RD) mimics several malignant, infectious, and inflammatory conditions [1]. IgG4-RD may present as Mikulicz’s disease, autoimmune pancreatitis, hypophysitis, Riedel thyroiditis, interstitial pneumonitis, interstitial nephritis, prostatitis, lymphadenopathy, retroperitoneal fibrosis, inflammatory aortic aneurysm, and other inflammatory states [2]. Until now, IgG4-RD has been considered rare in the West and exclusive to the Japanese and Korean population [3]. The exact pathological role of IgG4 antibodies underlying this disorder is not yet defined. The existence of the IgG4 subclass, with enhanced production of anti-inflammatory factors including production of IL-10 and other anti-inflammatory cytokines may help the immune system to dampen inappropriate inflammatory response, and IgG4 in IgG4-RD may not be responsible for the inflammatory reaction [4]. The identification of an antigenic trigger, the implications of IgG4 antibodies for pathophysiology and the precise immunological mechanisms leading to fibrosis is still elusive [5].
| Case Report | ▴Top |
Here we present the case of a 55-year-old African-American female with past medical history significant for diabetes mellitus, hypertension, coronary artery disease and obesity. She presented with a chronic indurated, painful, hyper-pigmented skin lesion on her right thigh which measured 6 inches in diameter (Fig. 1a). Sarcoidosis was initially suspected, as a bilateral hilar prominence was noted in X-ray of the chest. After a period of follow-up, the patient presented with pain and tenderness over the lesion, which prompted a referral to the dermatologist. A biopsy of the thigh lesion revealed lymphoplasmacytic infiltrate with positive immunohistochemistry staining for IgG4 (Fig. 2a, b). Her serum IgG4 level was 65 mg/dL (normal range 4 - 86 mg/dL). A 24-h urine collection contained 1 g of protein of glomerular type, secondary to long-standing diabetic nephropathy. There was no evidence of peripheral lymphadenopathy. CT of chest, abdomen and pelvis did not show evidence of mediastinal lymphadenopathy, hepatosplenomegaly, retroperitoneal lymphadenopathy or fibrosis. Initially, she was treated with prednisone. After 3 months of treatment with prednisone, significant resolution was achieved (Fig. 1b). However, the lesions recurred after discontinuing steroid therapy. At this time, she began treatment with four weekly courses of rituximab. Six weeks after the last dose of rituximab, near complete clearance of the lesion was noted. Four months after completing rituximab treatment, the lesions reappeared at the same site. She then received imuran with no appreciable benefit. Presently, she is on mycophenolate mofetil and is in remission.
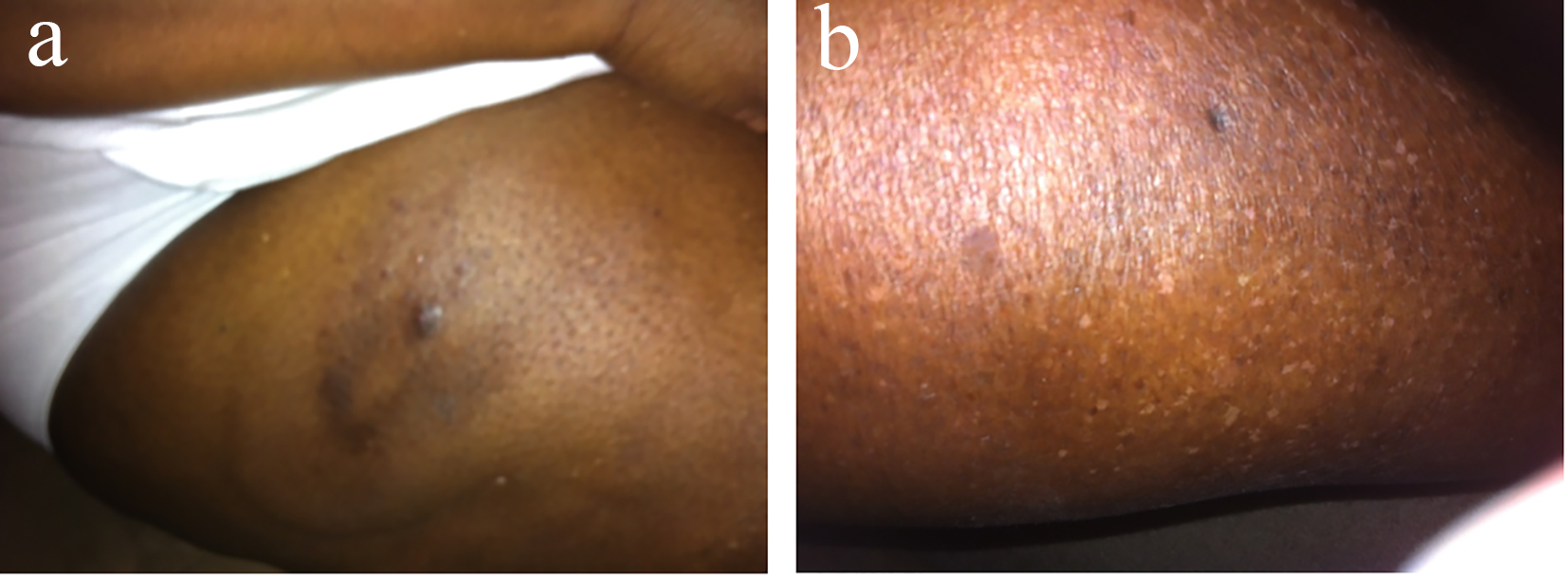 Click for large image | Figure 1. (a, b) Lesion in thigh 6 inches in diameter before and after treatment with prednisone. |
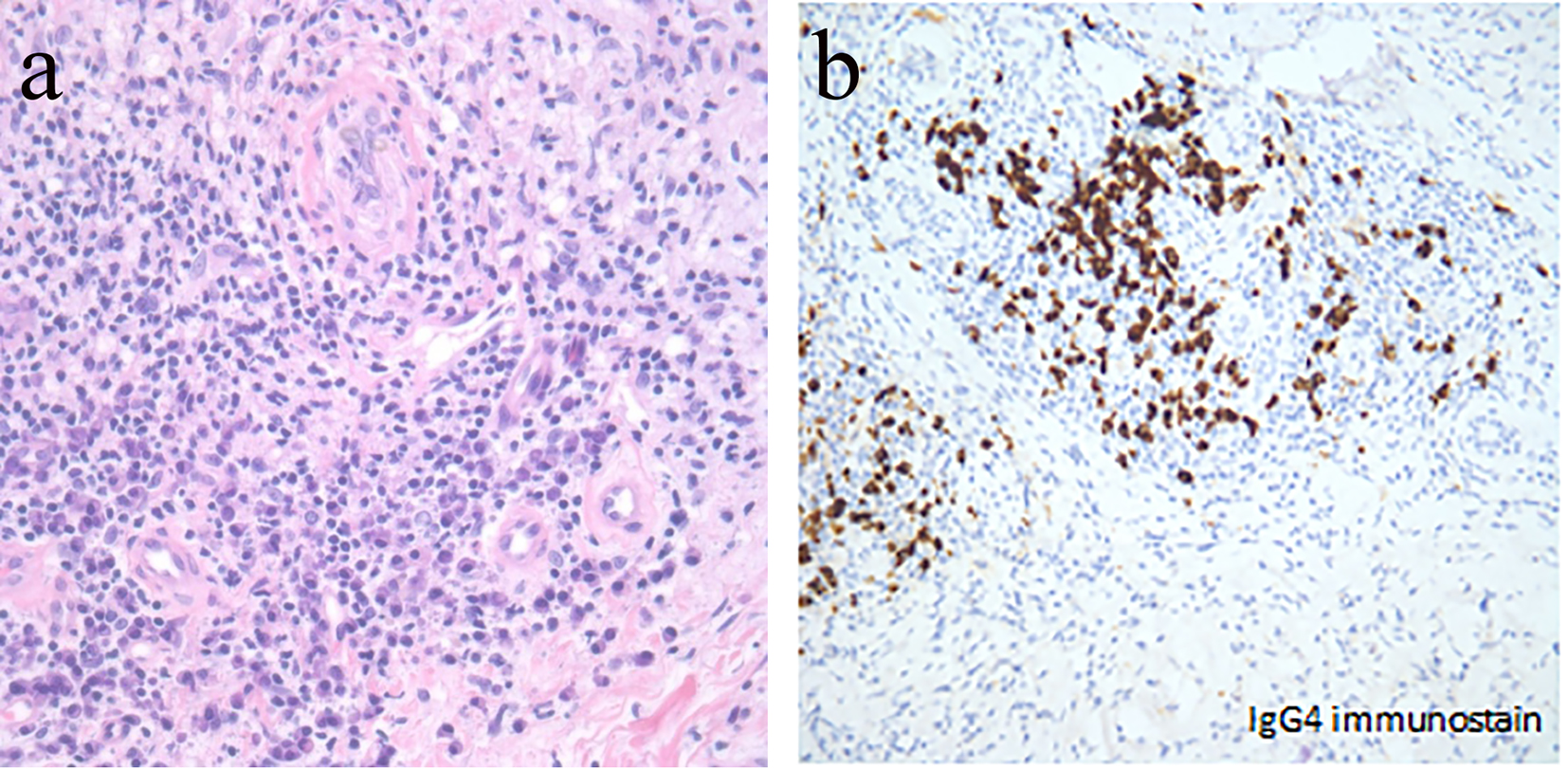 Click for large image | Figure 2. (a, b) H&E and immunohistochemistry staining of the skin lesion. |
| Discussion | ▴Top |
Unlike IgG1, IgG4 antibody is unable to participate in a tissue-destruction, but is associated with an inflammatory immune response [6]. IgG4-RD produces inflammatory response involving salivary glands, periorbital tissues, kidneys, lungs, lymph nodes, meninges, aorta, breast, prostate, thyroid, pericardium and the biliary system [7]. In addition to lymphoplasmacytic infiltrate with predominance of IgG4-positive plasma cells, IgG4-RD is associated with fibrosis. In IgG4-RD, regulatory T helper 2 cell-derived cytokines appear to contribute to the pathogenesis of the disease [8]. The structural basis for this abnormal behavior of IgG4 seems to be secondary to substitution of a single amino acid substitution of proline in core hinge of IgG1 to serine, altering configuration of IgG molecule [9]. This has a bearing on the management, as immunomodulatory therapy is the mainstay in the treatment IgG4-RD. A study from Japan showed that IgG4 levels fail to normalize in 63% of patients treated with glucocorticoids [10]. Our patient showed a relapsing course, following treatment with prednisone and other immunosuppressive agents consistent with literature presented by Kamisawa et al [11]. After recurrent relapses and exposure to immunosuppressive agents, non-Hodgkin lymphoma developed in about 3% during the follow-up of 3 - 5 years, suggesting that patients with IgG4-RD may be at an increased risk of secondary malignancy [12]. A review of the current literature suggests that our case is a previously unrecognized manifestation of IgG4-RD presenting as an indurated skin lesion with normal IgG4 levels. This case and variable nature of the disease illustrate the need for high index of suspicion to diagnose IgG4-RD.
Acknowledgments
We would like to thank Paul Rodriguez, MD, PhD, Dermatopathologist, University of South Florida for the photomicrographs.
Conflicts of Interest
Authors report no conflicts of interest.
| References | ▴Top |
- Kamisawa T, Zen Y, Pillai S, Stone JH. IgG4-related disease. Lancet. 2015;385(9976):1460-1471.
doi - Umehara H, Okazaki K, Masaki Y, Kawano M, Yamamoto M, Saeki T, Matsui S, et al. A novel clinical entity, IgG4-related disease (IgG4RD): general concept and details. Mod Rheumatol. 2012;22(1):1-14.
doi pubmed - Tuttolomondo A, Simonetta I, Di Raimondo D, Conigliaro R, Corpora F, Vassallo V, Pinto A. A Case Report of IgG4-related Syndrome and Literature Review. Curr Pharm Des. 2016.
doi - Aalberse RC, Stapel SO, Schuurman J, Rispens T. Immunoglobulin G4: an odd antibody. Clin Exp Allergy. 2009;39(4):469-477.
doi pubmed - Della-Torre E, Lanzillotta M, Doglioni C. Immunology of IgG4-related disease. Clin Exp Immunol. 2015;181(2):191-206.
doi pubmed - van der Zee JS, van Swieten P, Aalberse RC. Inhibition of complement activation by IgG4 antibodies. Clin Exp Immunol. 1986;64(2):415-422.
pubmed - Kamisawa T, Funata N, Hayashi Y, Eishi Y, Koike M, Tsuruta K, Okamoto A, et al. A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol. 2003;38(10):982-984.
doi pubmed - Koike T. IgG4-related disease: why high IgG4 and fibrosis? Arthritis Res Ther. 2013;15(1):103.
doi pubmed - Aalberse RC, Schuurman J. IgG4 breaking the rules. Immunology. 2002;105(1):9-19.
doi - Sah RP, Chari ST. Serologic issues in IgG4-related systemic disease and autoimmune pancreatitis. Curr Opin Rheumatol. 2011;23(1):108-113.
doi pubmed - Kamisawa T, Shimosegawa T, Okazaki K, Nishino T, Watanabe H, Kanno A, Okumura F, et al. Standard steroid treatment for autoimmune pancreatitis. Gut. 2009;58(11):1504-1507.
doi pubmed - Takahashi N, Ghazale AH, Smyrk TC, Mandrekar JN, Chari ST. Possible association between IgG4-associated systemic disease with or without autoimmune pancreatitis and non-Hodgkin lymphoma. Pancreas. 2009;38(5):523-526.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


