| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Case Report
Volume 5, Number 3, September 2016, pages 103-105
Agranulocytosis Secondary to Ceftaroline Use: A Case Report and Review of the Literature
Pooja Phulla, c, Adam Lernerb
aDepartment of Medicine, Boston University School of Medicine, Boston, MA, USA
bSection of Hematology/Oncology, Boston University School of Medicine, Boston, MA, USA
cCorresponding Author: Pooja Phull, Department of Medicine, Boston University School of Medicine, 72 East Concord Street, Evans 124, Boston, MA 02118, USA
Manuscript accepted for publication June 17, 2016
Short title: Agranulocytosis due to Ceftaroline Use
doi: http://dx.doi.org/10.14740/jh281w
| Abstract | ▴Top |
Ceftaroline is a fifth generation cephalosporin with bactericidal activity against both gram-negative and gram-positive organisms, and is the only cephalosporin with activity against methicillin-resistant Staphylococcus aureus (MRSA). A 23-year-old female with a history of frequent intravenous drug use was admitted to the medical intensive care unit with an MRSA infection resulting in bacterial meningitis, bacteremia and multifocal pneumonia. MRSA therapy was escalated during the admission to a combination of daptomycin and ceftaroline with subsequent clearance of her blood cultures. However, following the introduction of these medications, the patient developed agranulocytosis without parallel involvement of her other cell lines. This agranulocytosis resolved with discontinuation of ceftaroline. Clinicians must maintain vigilance with regard to patients’ neutrophil counts when prescribing treatment with ceftaroline for prolonged periods of time.
Keywords: Neutropenia; Agranulocytosis; Ceftaroline
| Introduction | ▴Top |
Ceftaroline is a fifth generation cephalosporin that is bactericidal for both gram-negative and gram-positive organisms [1]. It is distinguished from its fellow beta-lactam antibiotics by its high binding affinity for PBP-2a, which confers its bactericidal activity against methicillin-resistant Staphylococcus aureus (MRSA) [2]. Neutropenia, defined as clinically significant with an absolute neutrophil count (ANC) < 1,500 K/UL, has previously been associated with the cephalosporin class of antibiotics [3]. Patients with neutropenia are rendered immunodeficient, and predisposed to potentially fatal infections in a manner proportional to the degree of neutropenia [1]. This case report supports vigilance when treating patients with ceftaroline given the potential occurrence of this life-threatening side effect.
| Case Report | ▴Top |
Clinical course
A 23-year-old female with active intravenous drug abuse was admitted to the medical intensive care unit presenting with a 6-day history of dyspnea, malaise and progressively worsening diffuse pain. Her initial presentation was consistent with sepsis and blood cultures confirmed high-grade staphylococcal bacteremia. Imaging and a lumbar puncture revealed bacterial meningitis, multifocal pneumonia and a prevertebral abscess. Although endocarditis was ruled out with transesophageal echocardiogram, she was found to have endovascular disease with both a central venous sinus thrombosis and a thrombus within the right external jugular vein.
On admission, the patient’s white blood cell count was 7,600 K/UL with a left-shift (81% polymorphonuclear cells and 12% bands). The remainder of her complete blood count (CBC) showed an anemia of unknown chronicity (hemoglobin 8.9 g/dL) and a platelet count within the normal range. Although she was initially treated with vancomycin, ampicillin and meropenem, meropenem and ampicillin were discontinued 1 day after admission after blood cultures returned positive for Staphylococcus aureus. Given persistently positive blood cultures over the first 5 days of hospitalization, MRSA coverage was escalated from vancomycin to a combination of daptomycin and ceftaroline on hospital day 6. The patient responded favorably to this regimen, with negative blood cultures from hospital day 9 onwards. Neutropenia was first observed on hospital day 21 (ANC 1,300 K/UL). On hospital day 22, the patient’s ANC was 0. The remainder of her blood counts at that time revealed stable anemia and a rising platelet count. On retrospective review of her hematologic course, it was apparent that her ANC had steadily declined since the initiation of the escalated MRSA antibiotic regimen (Fig. 1). HIV serologies were negative. Review of a peripheral blood smear showed thrombocytosis and extremely rare polymorphonuclear neutrophils indicative of true neutropenia.
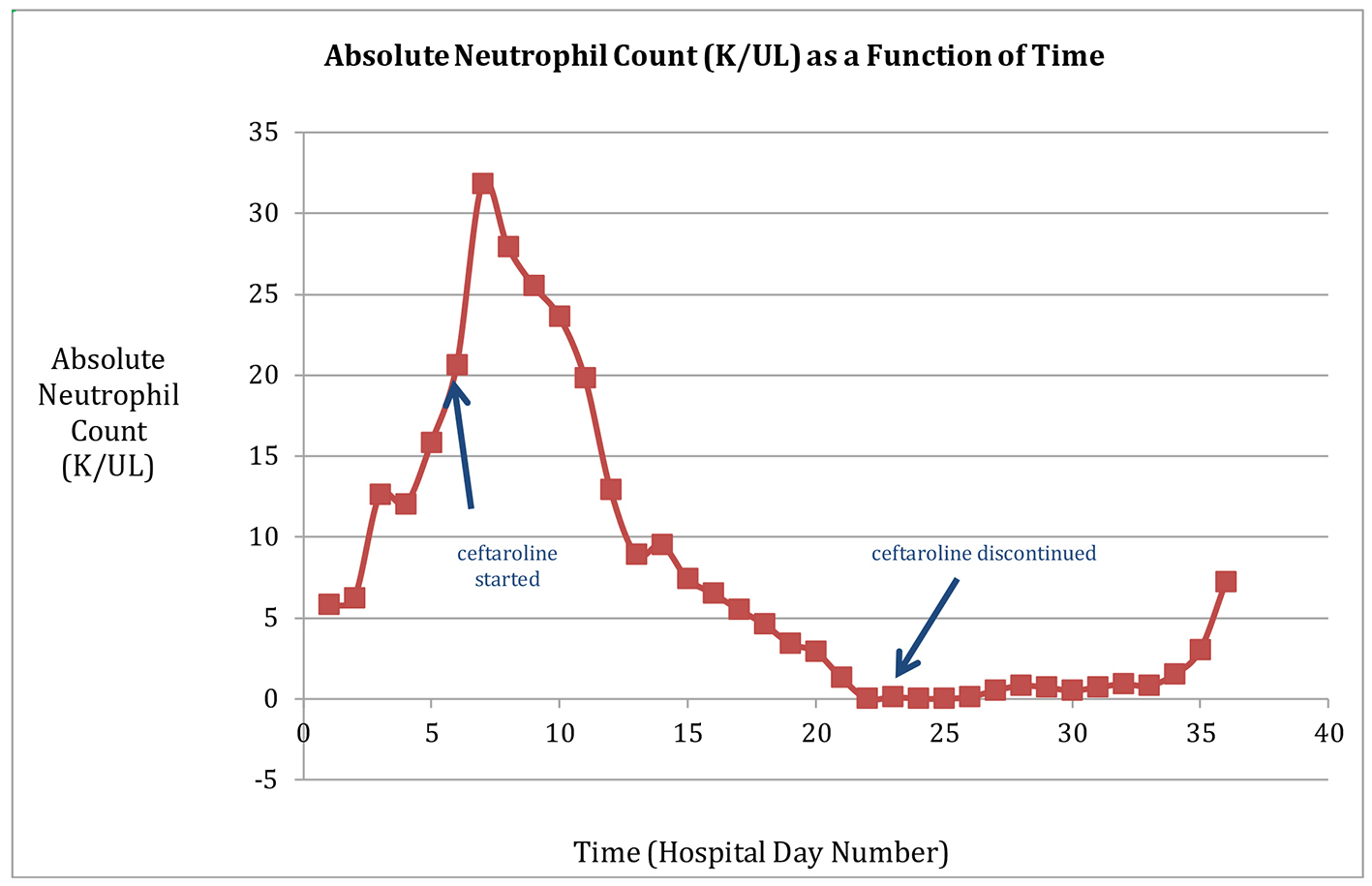 Click for large image | Figure 1. The patient’s ANC is depicted as a function of time, with the initiation and discontinuation of ceftaroline indicated by arrows. The time course reveals a gradual decline in ANC after ceftaroline therapy was introduced, and a subsequent recovery of ANC to the normal range after ceftaroline was discontinued. |
Treatment
Ceftaroline was discontinued on hospital day 22. Administration of granulocyte-colony stimulating factor (G-CSF) was considered, but was held in order to identify a possible response to discontinuation of ceftaroline. The patient did not develop complications from her agranulocytosis nor from cessation of ceftaroline therapy as of her date of discharge on hospital day 36.
Outcome and follow-up
After discontinuation of ceftaroline, the patient’s ANC remained at or below 500 K/UL for 5 days. Six days after discontinuation, her ANC increased to 800 K/UL. Eleven days after discontinuing ceftaroline, her ANC rose to the normal range and remained normal thereafter (Fig. 1). Given this improvement, bone marrow biopsy and G-CSF therapy were felt to be unnecessary. The patient was discharged with a central venous catheter for planned completion of a 6-week course of daptomycin alone.
| Discussion | ▴Top |
Ceftaroline is the only cephalosporin with activity against MRSA. It first received FDA approval for the treatment of community-acquired bacterial pneumonia and skin and soft tissue infections in October of 2010 [4]. Neutropenia has previously been associated with the cephalosporin class of antibiotics. While the mechanism of this side effect has not been fully elucidated, several studies have postulated drug-induced maturation arrest of bone marrow [5] or an immunologically-mediated process as possible explanations of this phenomenon [6].
A PubMed search using the keywords “ceftaroline” and “neutropenia” identified nine publications, four of which were relevant to this topic [1, 3, 5, 7]. All of these studies confirmed an association between long-term ceftaroline therapy and the development of neutropenia. The largest study, a retrospective cohort analysis conducted in an academic medical center over a 30-month period, identified 39 patients treated with ceftaroline for more than 7 days. Seven of these patients developed clinically significant neutropenia, which correlates to an incidence of 18% based on this analysis [1]. The median number of days required for the development of neutropenia was 17. These findings are consistent with the patient discussed in this case report, whose neutropenia was first observed on day 16 of ceftaroline therapy [1]. The authors were able to collect follow-up data on 71% of the patients who became neutropenic while on ceftaroline; all such patients experienced complete recovery of their neutrophil counts with cessation of ceftaroline therapy [1]. The ANC returned to normal within 14 days in the majority of these patients [1]. Similarly, the ANC of the patient featured in this report returned to normal within 11 days of cessation of ceftaroline therapy.
Ceftaroline is an important option for the treatment of antibiotic-resistant microbial strains. The findings reported in this case, however, provide a reminder of the risks of use of this agent for longer than a 2-week period. As previously recommended by others, careful monitoring of neutrophil counts is indicated in patients treated with this antibiotic for prolonged periods.
Acknowledgments
The authors would like to thank Faisal Rahman, MD, who assisted in revising the manuscript.
Competing Interests
The authors have no competing interests.
Author Contributions
PP participated in collection and interpretation of data, drafting and revising the manuscript, read and approved the final manuscript. AL reviewed, edited, and approved the final manuscript.
Abbreviations
MRSA: methicillin-resistant Staphylococcus aureus; ANC: absolute neutrophil count; CBC: complete blood count; G-CSF: granulocyte-colony stimulating factor
| References | ▴Top |
- LaVie KW, et al. Neutropenia associated with long-term ceftaroline use. Antimicrobial Agents and Chemotherapy 2015; 60(1): 264-269.
doi pubmed - Girish C, Balakrishnan S. Ceftaroline fosamil: A novel anti-Methicillin-resistant Staphylococcus aureus cephalosporin. J Pharmacol Pharmacother. 2011;2(3):209-211.
doi pubmed - Rimawi RH, Frenkel A, Cook PP. Ceftaroline - a cause for neutropenia. J Clin Pharm Ther. 2013;38(4):330-332.
doi pubmed - File TM, Jr., Wilcox MH, Stein GE. Summary of ceftaroline fosamil clinical trial studies and clinical safety. Clin Infect Dis. 2012;55(Suppl 3):S173-180.
doi pubmed - Yam FK, Kwan BK. A case of profound neutropenia and agranulocytosis associated with off-label use of ceftaroline. Am J Health Syst Pharm. 2014;71(17):1457-1461.
doi pubmed - Uy N, Thiagarajan P, Musher DM. Cephalosporin side chain idiosyncrasies: a case report of ceftriaxone-induced agranulocytosis and review of literature. Open Forum Infect Dis. 2015;2(1):ofv007.
doi pubmed - Varada NL, Sakoulas G, Lei LR, Chua J. Agranulocytosis with ceftaroline high-dose monotherapy or combination therapy with clindamycin. Pharmacotherapy. 2015;35(6):608-612.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


