| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Review
Volume 1, Number 2-3, June 2012, pages 39-43
Musculo-Skeletal Complications of Hemophilia
E. Carlos Rodriguez-Merchan
Department of Orthopaedic Surgery, La Paz University Hospital, Paseo de la Castellana 261, 28046-Madrid, Spain
Manuscript accepted for publication June 12, 2012
Short title: MS Complications of Hemophilia
doi: https://doi.org/10.4021/jh18e
- Abstract
- Introduction
- Hemarthrosis
- Chronic Synovitis
- Articular Deformities, Subchondral Cysts and Osteophytes
- Advanced Arthropathy
- Pseudotumors
- HIV-Positive Patients
- Conclusion
- References
| Abstract | ▴Top |
Prophylactic treatment from ages 2 to 18 years could avoid the development of hemophilic arthropathy if the concentration of the patient’s deficient factor is prevented from falling below 1% of normal. A review of the literature on the musculo-skeletal complications of hemophilia has been performed. Early treatment is of paramount importance because the immature skeleton is very sensitive to the complications of hemophilia; severe structural deficiencies may develop quickly. Major hemarthrosis (including joint aspiration) and chronic hemophilic synovitis should be treated aggressively to prevent hemophilic arthropathy. For the treatment of chronic haemophilic synovitis, radiosynovectomy should always be indicated as the first procedure. If, after three procedures with 6-month interval, radiosynovectomy fails, an arthroscopic synovectomy must be indicated. When advanced hemophilic arthropathy is present with severe disability, the aim should be to restore function. Arthroscopic joint debridement is an effective method to achieve this goal and can be considered to be an alternative to total joint arthroplasty in the younger age groups. Finally total joint arthroplasty can usually be relied upon to restore both mobility and function in a diseased joint. The potential benefits of joint arthroplasty must though always be weighed up against the long term sequelae, especially loosening and consequent revision surgery. A correct surgical haemostasis must be achieved by the infusion of factor concentrate at the right dose. Prophylactic treatment from ages 2 to 18 years could avoid the development of hemophilic arthropathy if the concentration of the patient’s deficient factor is prevented from falling below 1% of normal. Major hemarthrosis, chronic hemophilic synovitis and the initial stages of hemophilic arthropathy should be treated aggressively to prevent hemophilic arthropathy. Finally total joint arthroplasty can usually be relied upon to restore both mobility and function in a diseased joint. A correct surgical haemostasis must be achieved by the infusion of factor concentrate at the right dose.
Keywords: Haemophilia; Musculo-skeletal; Complications
| Introduction | ▴Top |
The articular problems of hemophilic patients begin in infancy. These include: recurrent hemarthrosis, chronic synovitis, flexion deformities, hypertrophy of the growth epiphyses, damage to the articular cartilage and destruction of the joint (hemophilic arthropathy). The most commonly affected joints are the ankle, the knee, the elbow and the hip. The hemarthrosis tend to persist despite the reabsortive properties of the synovium which eventually becomes hypertrophic and more prone to injury, leading to a vicious circle of bleeding, synovitis and more bleeding. The pain causes flexion deformities in affected joints, first correctable, but later becoming fixed. The hyperemic reaction to the hemarthrosis produces hypertrophy of the growth epiphyses. This is often asymmetrical, producing a valgus deformity at the involved joint. Both factors lead to damage to the articular cartilage, which evolves into the destruction of the joint (hemophilic arthropathy) [1, 2] (Fig. 1).
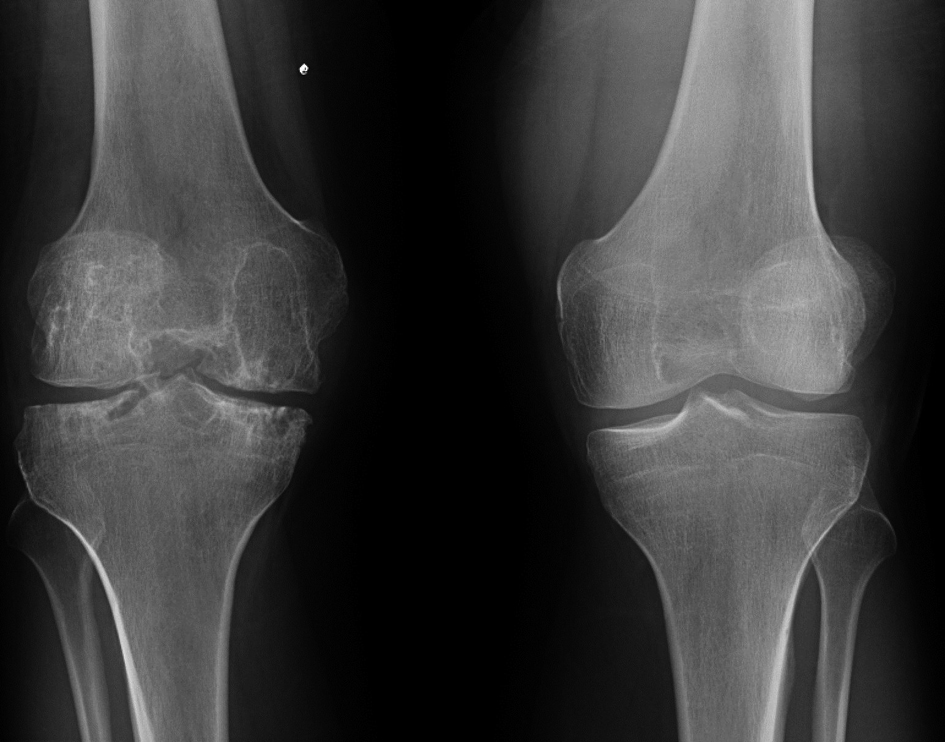 Click for large image | Figure 1. Right knee joint involvement in a hemophilic patient after recurrent bleeding episodes. Note the contralateral healthy knee for comparison. |
| Hemarthrosis | ▴Top |
The correct management of hemophilic hemarthrosis should include: prompt diagnosis, adequate hematological treatment, joint aspiration, physiotherapy and avoidance of re-bleeding. Patients with hemarthrosis commonly feel a tingling sensation- the ‘aura’- before the episode of intra-articular bleeding. The joint becomes warm, swollen, very painful and with an antialgic position in flexion. Clinical diagnosis should be confirmed by means of ultrasonography. Radiographs should also be performed, looking for any evidence of radiological involvement. Until recently hemarthrosis have been treated by means of intravenous injection of 20 - 30 U/kg body weight of the deficient coagulation factor under hematological control, short-term rest and immobilization in the antialgic position by means of bandages, plaster splints, bed rest, and analgesics. Only 20% of the countries around the world have sufficient economical power to give their hemophilia population on-demand substitutive therapy. This consists of the intravenous injection of 20 - 30 units of Factor VIII/kg body weight when a bleed occurs, until the symptoms of an acute hemarthrosis abate [3].
Today, I believe on the efficacy of early joint aspiration. However, the technique must be performed under hematological control and aseptic conditions. The procedure must be repeated many times in the patient’s life, starting at a very short age, and it carries some difficulties; therefore, psychological and familiar supports are paramount. It is important that the child trusts the orthopedic surgeon carrying out the joint aspiration and some form of local anesthesia should be used in order to minimize pain. Following the procedure, immobilization is recommended for 3 - 5 days by means of a compressive bandage. Later on, the patient should start a supervised period of physiotherapy as rehabilitation is paramount to halt the development of synovitis. The duration of physiotherapy will depend on the time required to regain full range of movement and muscular strength. Re-bleedings during the recovery period should be avoided as much as possible. Patients must be seen every 3 months at the outpatient clinic for close and careful assessment [4].
| Chronic Synovitis | ▴Top |
The objectives of treatment are to stop the hemarthrosis or to control them quickly and to avoid secondary synovitis. Once synovitis has developed, which is inevitable, the aim is to treat it as early and aggressively as possible. Confirmation of the diagnosis is important and can be achieved by ultrasound or MRI (Fig. 2). Sometimes standard conservative measures, such as factor replacement and physiotherapy, do not break the vicious cycle of hemarthrosis-synovitis-hemarthrosis. Under these circumstances synovectomy-either chemical, radioactive or surgical (open or arthroscopic) can reduce the bleeding tendency and so delay the onset of hemophilic arthropathy.
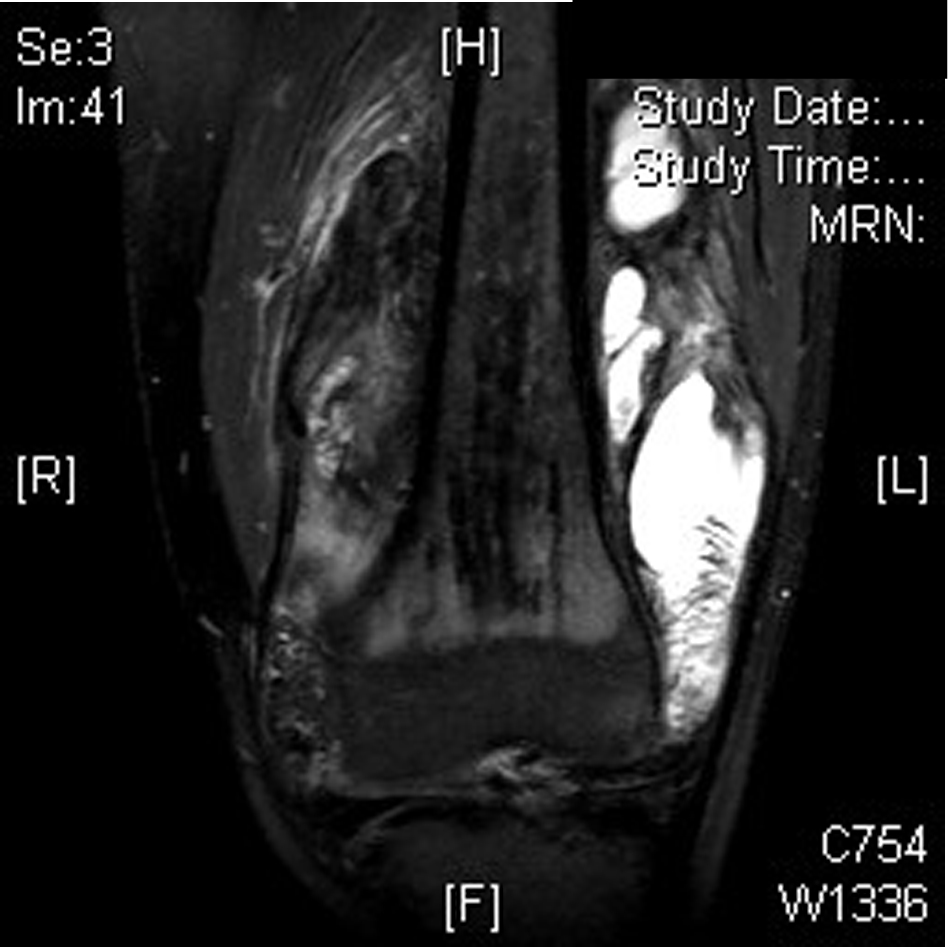 Click for large image | Figure 2. Advanced hemophilic arthropathy of the knee in a young person with hemophilia (MRI). |
Currently we perform ablation of the synovium as soon as synovitis is diagnosed. There are both conservative (medical synovectomy) and operative methods (arthroscopic synovectomy). The procedure of injection into the joint is termed medical synovectomy; the drugs most commonly used are rifampicin and radioactive isotopes such as Yttrium-90, Rhenium-186 and Phosphorus-32 [5-7]. In my experience, synovectomy (by any method) reduces the tendency to bleeding episodes, but does not halt the deterioration of joints. Radiosynovectomy (RS) should be the first choice for patients with persistent synovitis of the joints. If three consecutive RSs at 6 month intervals fail to halt synovitis, a surgical artrhroscopic synovectomy should be considered as an alternative to the treatment of chronic hemophilic synovitis.
| Articular Deformities, Subchondral Cysts and Osteophytes | ▴Top |
As already stated, an uncontrolled hemarthrosis and synovitis will lead to flexion deformity, some times with valgus deviation caused by asymmetrical growth of the epiphyses, Pertheś disease, osteophytes and subchondral cysts. In infants, adolescents and young adults with flexion deformity, realignment osteotomies may be indicated to prevent development of severe arthropathy [8, 9]. Flexion deformities should be managed by early physiotherapy, traction, orthoses, tendon and capsular release, or extension osteotomy. Flexion deformity of the knee requires early physiotherapy and the use of progressive traction in extension and appropriate orthoses. If these conservative methods fail, hamstring release or supracondylar femoral extension osteotomy may be indicated.
At the hip, a form of Pertheś disease may develop related to recurrent intra-articular bleeding. The initial treatment should be by means of an ambulation-abduction bracing. Because of intraosseous hemorrhages, some hemophilic patients develop large symptomatic juxta-articular cysts, especially in the proximal tibia. These may threaten the integrity of the articular cartilage and require open curettage and grafting with the use of fibrin sealant [10]. At the ankle some patients develop a large anterior osteophyte; surgical excision (queilectomy) of this can give relief of symptoms [11].
| Advanced Arthropathy | ▴Top |
Between the second and fourth decades, many hemophiliacs develop severe articular destruction (Fig. 3). At this stage, possible treatments include arthroscopic debridement, arthrodesis (joint fusion) and total knee arthroplasty [3]. In polyarthritic conditions, the repair of a single joint may not improve functional ability, and the aim should be to create a functional limb. Horoszowski et al [12] reported the use of multiple joint procedures on hemophilic patients in a single operative session. This succeeded in achieving a functional limb. The complication rate was lower than expected and the rehabilitation period was relatively short.
 Click for large image | Figure 3. Hemophilic arthropathy of the ankle showing subchondral sclerosis, narrowing of the joint line and subchondral cysts (MRI). |
At the mature elbow, the resection of a hypertrophic radial head usually reduces the incidence of recurrent hemorrhages and improves the range of pronation-supination of the affected joint. For the hip the best solution is a total hip arthroplasty [3, 13, 14]. Converting a hip that is ankylosed to a total hip replacement commonly results in relief of pain in the lower back and knee, inproved mobility of the hip and correction of limb length discrepancy [3].
I advise arthroscopic debridement for painful knees in young patients, with long life expectancy, before considering total knee arthroplasty. When debridement fails or in older patients or those with a shorter life expectancy, a total knee arthroplasty should be advised (Fig. 4). In the era of total joint arthroplasties in orthopedics it is obvious that a total knee arthroplasty should be indicated in hemophilia patients suffering from severe knee pain and disability. However, the expected high risk of infection and other postoperative complications is a concern. The orthopedic surgeon should weigh up the risks and benefits carefully. Clinical and immunological status should be considered before suggesting total knee replacement to a hemophilia patient [3].
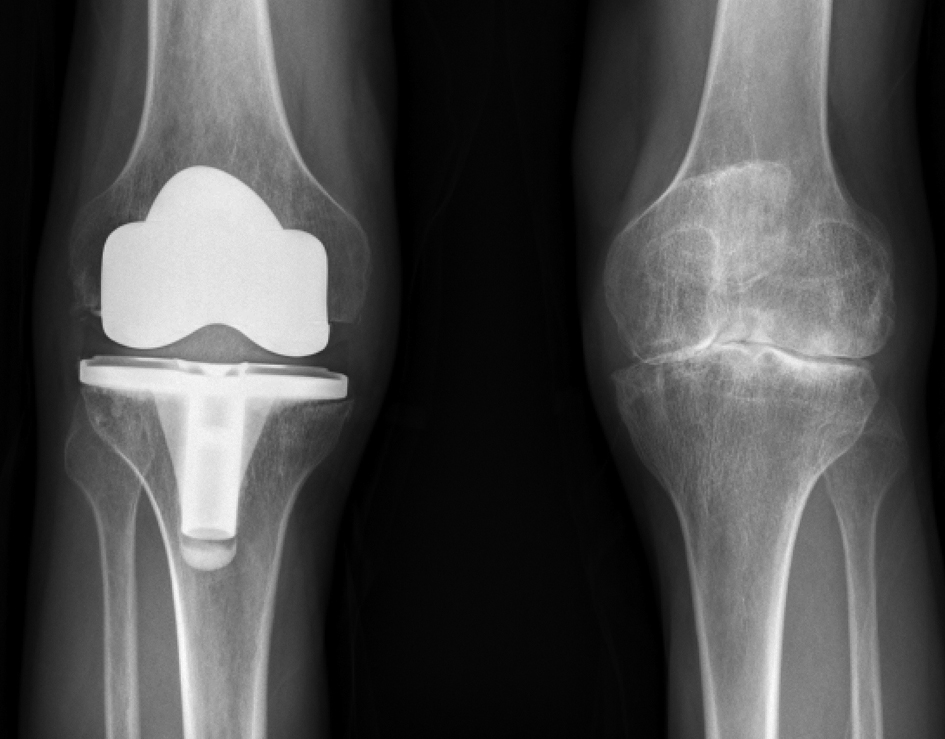 Click for large image | Figure 4. Left knee joint involvement in a hemophilic patient after recurrent bleeding episodes. The right knee had already required a total knee arthroplasty 5 years ago. |
It is my view that joint arthroplasties are surgical procedures with a high complication rate and an excessive risk of postoperative infection, particularly in HIV-positive hemophilia patients with CD4 counts of < 200. It must be remembered that approximately 80% of the hemophilia population in developed countries is HIV-positive, largely as a result of contaminated factor concentrates in the early 1980s. Given the existing risks of postoperative infection in the HIV-positive hemophilia patient, and the high rate of unsatisfactory results that have been reported, total joint arthroplasties are surgical procedures to be considered only for use in selected cases. Life expectancy, age and immunological status are factors paramount in the decision to proceed with a total joint arthroplasty in hemophilia.
Although arthroscopic debridement should not be looked upon as an alternative to total knee arthroplastry, it should be considered in the young hemophiliac to avoid, or delay, total knee arthroplasty. The operation may give the patient years of life without pain. When arthroscopic debridement fails to relieve pain, replacement must be considered. End-stage arthropathy of the ankle, with intractable pain, increasing or severe deformity and continued bleeding episodes are indications for arthrodesis or total ankle arthroplasty [3, 11].
| Pseudotumors | ▴Top |
Pseudotumor is a serious, but very rare complication. A progressive cystic swelling involving muscle is produced by recurrent bleeding and there is usually radiological evidence of bone involvement. Most are in adults near the large bones of the proximal skeleton. A few develop distal to the wrist and ankle in younger patients before skeletal maturity. Untreated proximal pseudotumors will destroy soft tissues, erode bone and produce vascular or neurological lesions.
Surgical removal is the treatment of choice, but should only be performed in major hemophilia centers, since it has a mortality rate of 20%. Some regression, but not true cure, may follow long-term replacement therapy and immobilization, but conservative treatment is not recommended except in patients with high-titer inhibitors for whom surgery is impossible. In such cases, percutaneous evacuation with filling by fibrin sealant or cancellous bone, depending on the size, may be helpful. Distal pseudotumors should be treated primarily by long-term factor replacement and cast immobilization; they tend to respond better to conservative management [3].
| HIV-Positive Patients | ▴Top |
The spread of human immunodeficiency virus in patients with hemophilia has led to an increasing incidence of septic arthritis, soft-tissue infection and increased risk of infection after orthopedic surgery not only for the patient but also for the surgical staff. The diagnosis of septic arthritis has often been delayed because the symptoms are similar to those of an acute hemarthrosis. It is important to remember that a painful and swollen joint, mimicking hemarthrosis, could be due to septic arthritis, especially when factor VIII replacement fails to relieve the symptoms and there is pyrexia. Immediate joint aspiration and culture are mandatory. Appropriate antibiotic therapy can be curative, but surgical drainage may be necessary [3, 15]. The knee is most commonly affected, followed by the elbow, but any joint may be involved. Staphylococcus aureus is the usual organism, but our review has shown that Salmonella may also be the cause. In factor VIII deficient patients, a positive HIV status is strongly related to septic arthritis and there is also a high risk of developing full-blown AIDS. Septic arthritis provides a clinical marker for immunodepression in hemophiliac patients.
A survey of hemophilia treatment centers in the USA by Ragni et al [16] determined the incidence of postoperative infection in HIV-positive hemophiliac patients with CD4 counts of 200 or less. Total joint arthroplasty appeared to have 10 times the risk of infection than other procedures. Orthopedic operations have a significantly higher rate of exposure to blood than other types of surgery.
| Conclusion | ▴Top |
In conclusion, prophylactic treatment from ages 2 to 18 years could avoid the development of hemophilic arthropathy if the concentration of the patient's deficient factor is prevented from falling below 1% of normal [17, 18]. Major hemarthrosis, chronic hemophilic synovitis and the initial stages of hemophilic arthropathy should be treated aggressively to prevent hemophilic arthropathy [3, 19-21]. Finally total joint arthroplasty can usually be relied upon to restore both mobility and function in a diseased joint [3, 13, 14, 22]. A correct surgical haemostasis must be achieved by the infusion of factor concentrate at the right dose [23].
| References | ▴Top |
- Luck JV, Jr., Silva M, Rodriguez-Merchan EC, Ghalambor N, Zahiri CA, Finn RS. Hemophilic arthropathy. J Am Acad Orthop Surg. 2004;12(4):234-245.
pubmed - Rodriguez-Merchan EC. Effects of hemophilia on articulations of children and adults. Clin Orthop Relat Res. 1996;328:7-13.
pubmed - Valentino LA, Hakobyan N, Rodriguez N, Hoots WK. Pathogenesis of haemophilic synovitis: experimental studies on blood-induced joint damage. Haemophilia. 2007;13 Suppl 3:10-13.
pubmed - Roosendaal G, Jansen NW, Schutgens R, Lafeber FP. Haemophilic arthropathy: the importance of the earliest haemarthroses and consequences for treatment. Haemophilia. 2008;14 Suppl 6:4-10.
pubmed - Rodriguez-Merchan EC, Quintana M, De la Corte-Rodriguez H, Coya J. Radioactive synoviorthesis for the treatment of haemophilic synovitis. Haemophilia. 2007;13 Suppl 3:32-37.
pubmed - Fernandez-Palazzi F. Treatment of acute and chronic synovitis by non-surgical means. Haemophilia. 1998;4(4):518-523.
pubmed doi - De la Corte-Rodriguez H, Rodriguez-Merchan EC, Jimenez-Yuste V. Radiosynovectomy in hemophilia: quantification of its effectiveness through the assessment of 10 articular parameters. J Thromb Haemost. 2011;9(5):928-935.
pubmed doi - Smith MA, Urquhart DR, Savidge GF. The surgical management of varus deformity in haemophilic arthropathy of the knee. J Bone Joint Surg Br. 1981;63-B(2):261-265.
pubmed - Pearce MS, Smith MA, Savidge GF. Supramalleolar tibial osteotomy for haemophilic arthropathy of the ankle. J Bone Joint Surg Br. 1994;76(6):947-950.
pubmed - Patel S, Rodriguez-Merchan EC, Haddad FS. The use of fibrin glue in surgery of the knee. J Bone Joint Surg Br. 2010;92(10):1325-1331.
pubmed doi - Ribbans WJ, Phillips AM. Hemophilic ankle arthropathy. Clin Orthop Relat Res. 1996;328:39-45.
pubmed - Horoszowski H, Heim M, Schulman S, Varon D, Martinowitz U. Multiple joint procedures in a single operative session on hemophilic patients. Clin Orthop Relat Res. 1996;328:60-64.
pubmed - Miles J, Rodriguez-Merchan EC, Goddard NJ. The impact of haemophilia on the success of total hip arthroplasty. Haemophilia. 2008;14(1):81-84.
pubmed - Lofqvist T, Sanzen L, Petersson C, Nilsson IM. Total hip replacement in patients with hemophilia. 13 hips in 11 patients followed for 1-16 years. Acta Orthop Scand. 1996;67(4):321-324.
pubmed doi - Gilbert MS, Aledort LM, Seremetis S, Needleman B, Oloumi G, Forster A. Long term evaluation of septic arthritis in hemophilic patients. Clin Orthop Relat Res. 1996;328:54-59.
pubmed - Ragni MV, Crossett LS, Herndon JH. Postoperative infection following orthopaedic surgery in human immunodeficiency virus-infected hemophiliacs with CD4 counts < or = 200/mm3. J Arthroplasty. 1995;10(6):716-721.
pubmed doi - Manco-Johnson MJ, Abshire TC, Shapiro AD, Riske B, Hacker MR, Kilcoyne R, Ingram JD, et al. Prophylaxis versus episodic treatment to prevent joint disease in boys with severe hemophilia. N Engl J Med. 2007;357(6):535-544.
pubmed doi - Oldenburg J. Prophylaxis in bleeding disorders. Thromb Res. 2011;127 Suppl 1:S14-17.
pubmed - Rodriguez-Merchan EC, Magallon M, Galindo E, Lopez-Cabarcos C. Hemophilic synovitis of the knee and the elbow. Clin Orthop Relat Res. 1997;343:47-53.
pubmed - Rodriguez-Merchan EC. The haemophilic ankle. Haemophilia. 2006;12(4):337-344.
pubmed doi - Verma N, Valentino LA, Chawla A. Arthroscopic synovectomy in haemophilia: indications, technique and results. Haemophilia. 2007;13 Suppl 3:38-44.
pubmed - Rodriguez-Merchan EC. Aspects of current management: orthopaedic surgery in haemophilia. Haemophilia. 2012;18(1):8-16.
pubmed doi - Scharrer I. Experience with KOGENATE Bayer in surgical procedures. Haemophilia. 2002;8 Suppl 2:15-18.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.


