Figures
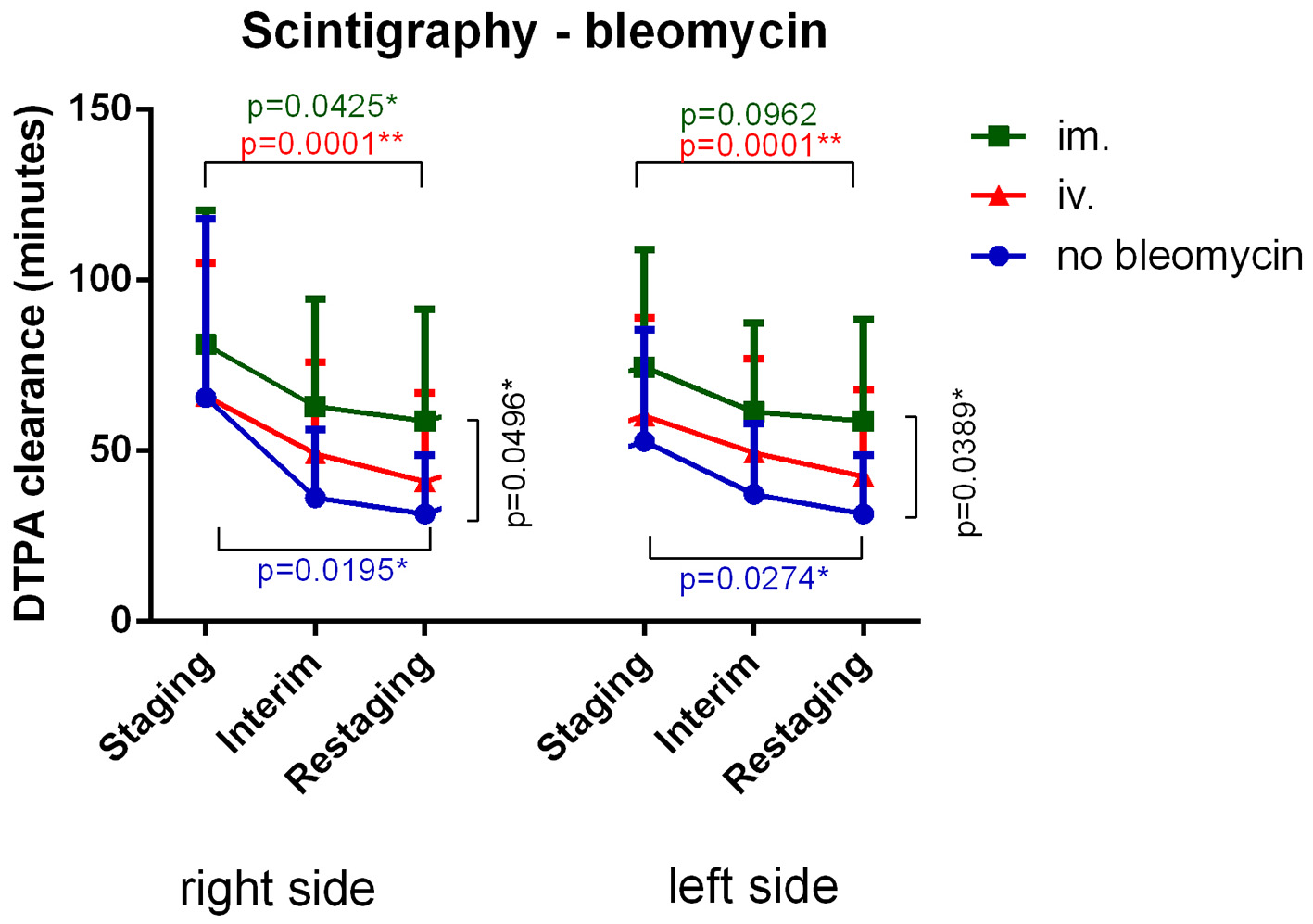
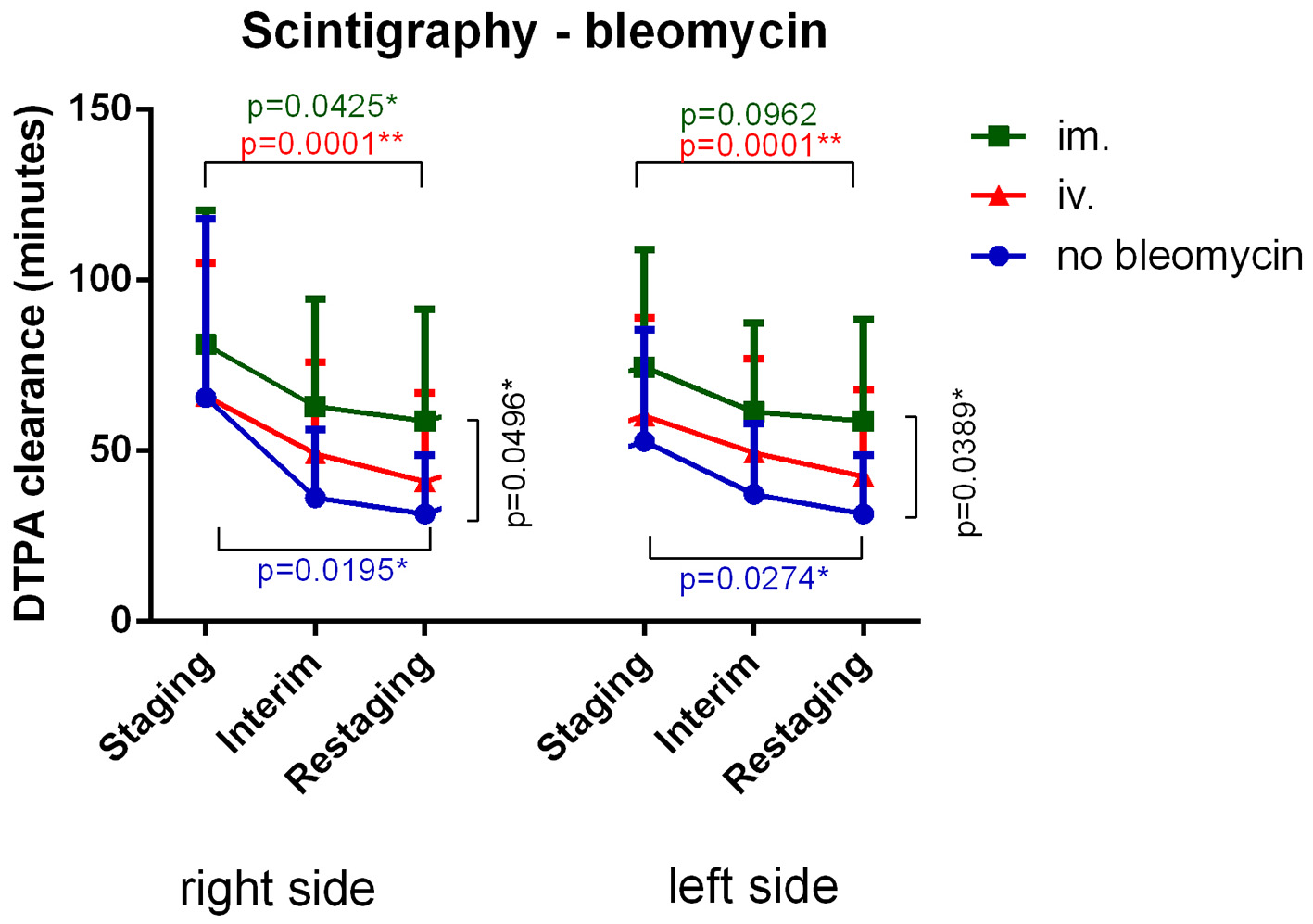
Figure 1. Intravenous bleomycin administration most significantly decreased DTPA clearance versus baseline. Intramuscular bleomycin administration lessened DTPA clearance decline. Patients who were not given bleomycin still experienced a significant decrease in DTPA clearance. DTPA: diethylenetriamine pentaacetic acid; IM: intramuscular; IV: intravenous.
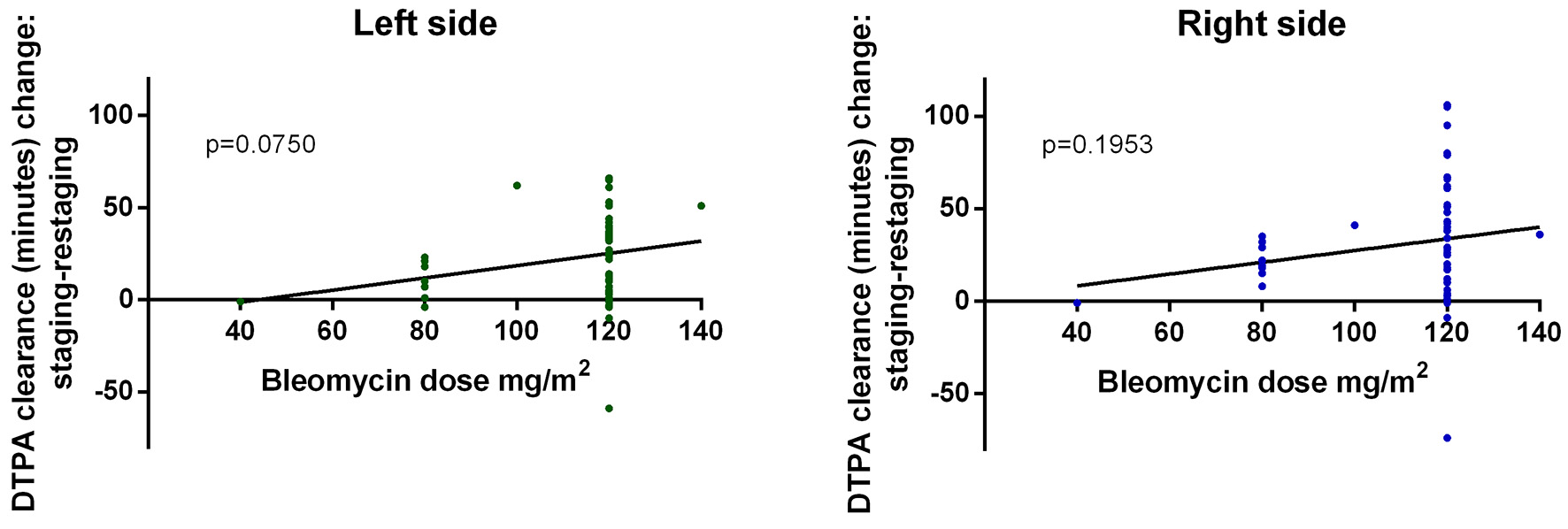
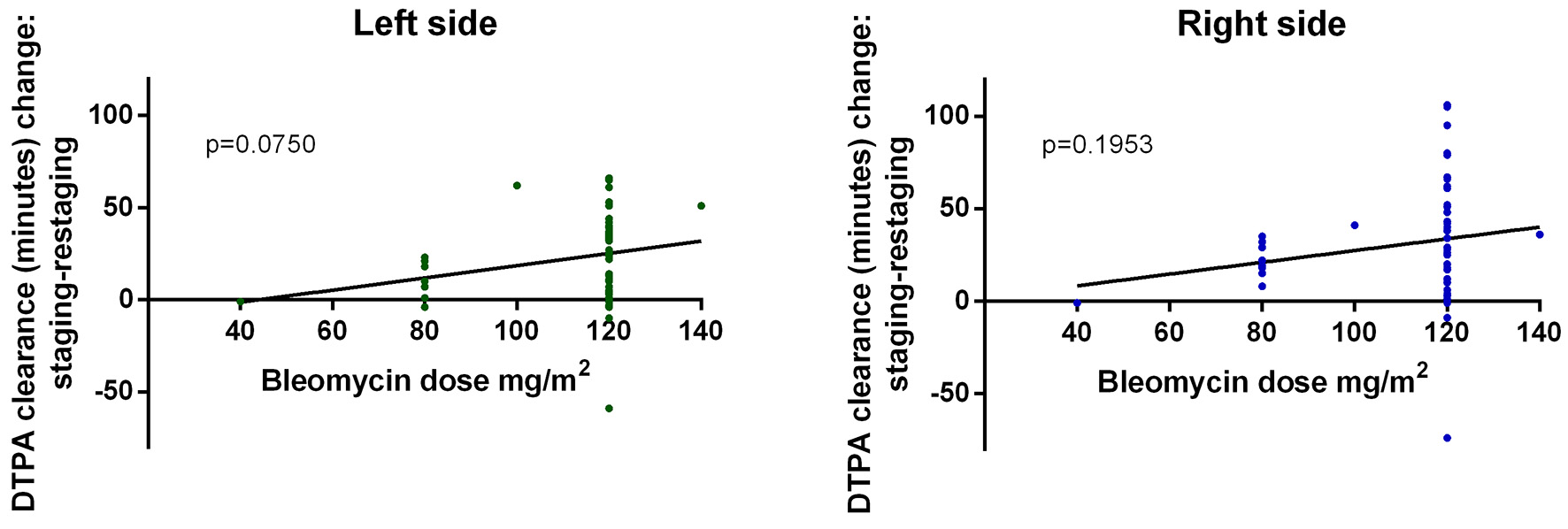
Figure 2. Scintigraphy results continuously worsened as cumulative bleomycin dose increased. DTPA: diethylenetriamine pentaacetic acid.
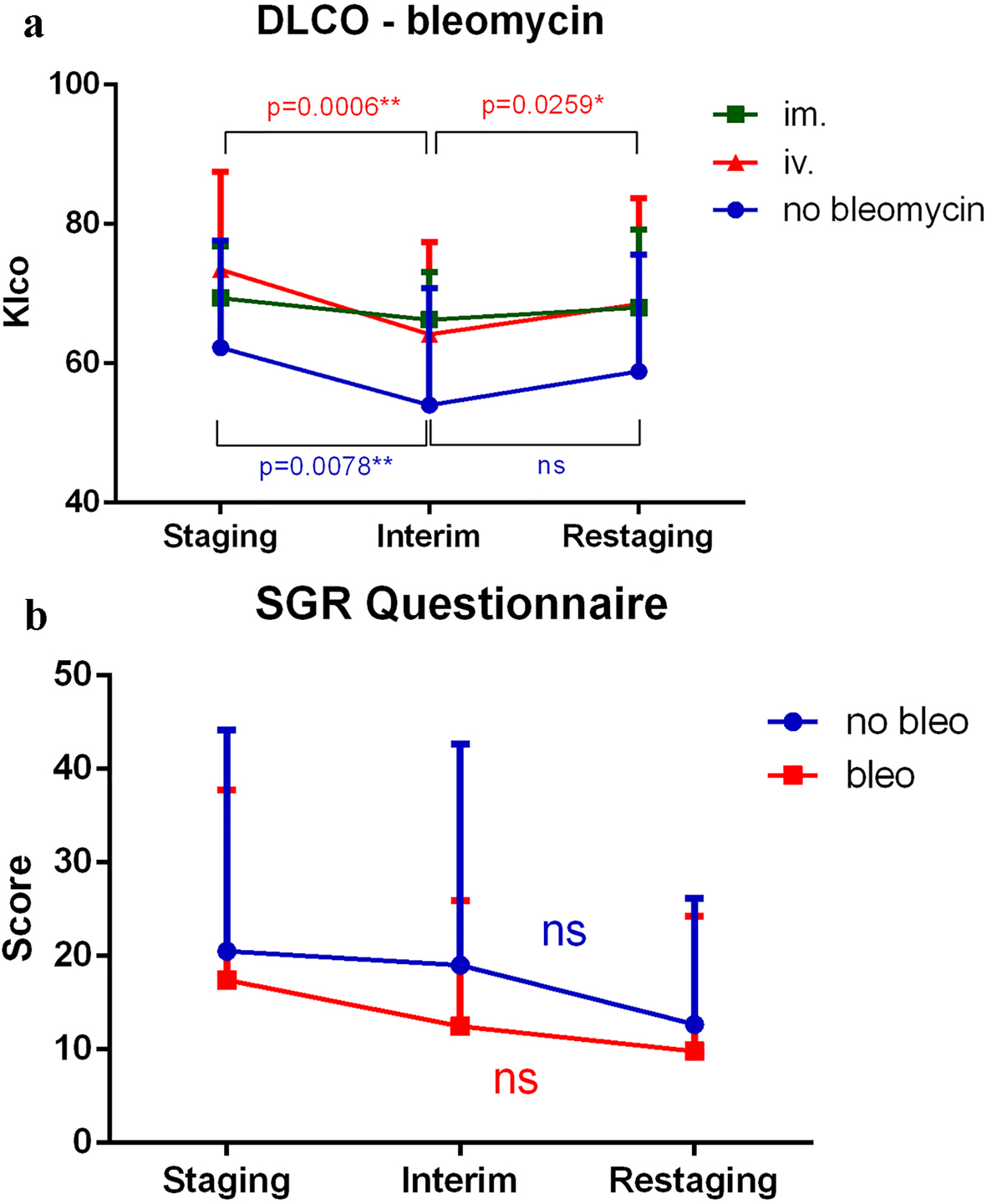
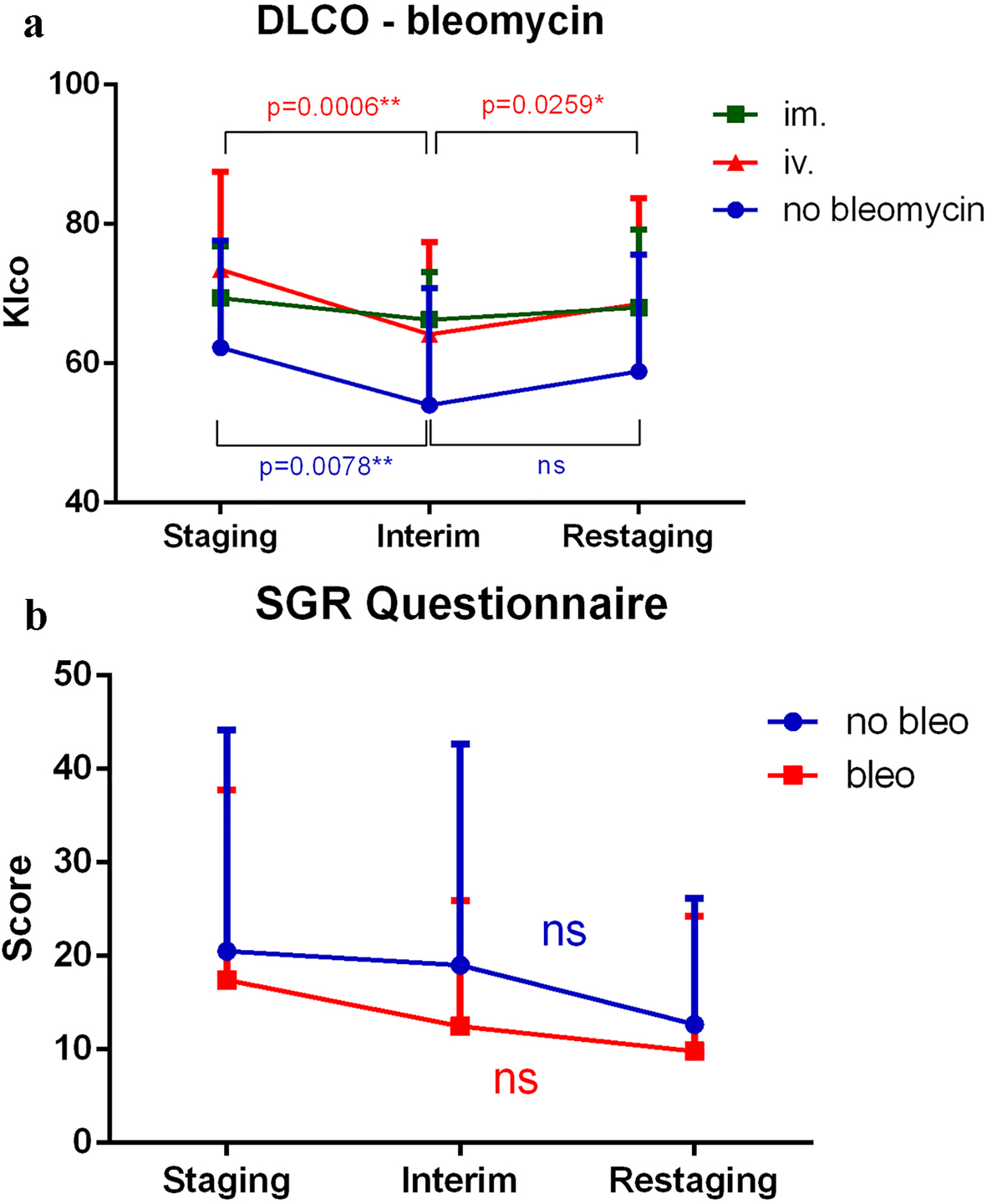
Figure 3. (a) DLCO significantly worsened between staging and interim time points when all treatment modalities were applied except intramuscular administration; however, pulmonary function normalized by the restaging time point. (b) SGRQ scores decreased, and therefore, subjective patient symptoms generally improved throughout treatment. However, the differences were not significant. SGRQ: St. George Respiratory Questionnaire; DTPA: diethylenetriamine pentaacetic acid; DLCO: carbon monoxide diffusion capacity of the lung; Klco: transfer coefficient of the lung for carbon monoxide; IM: intramuscular; IV: intravenous.
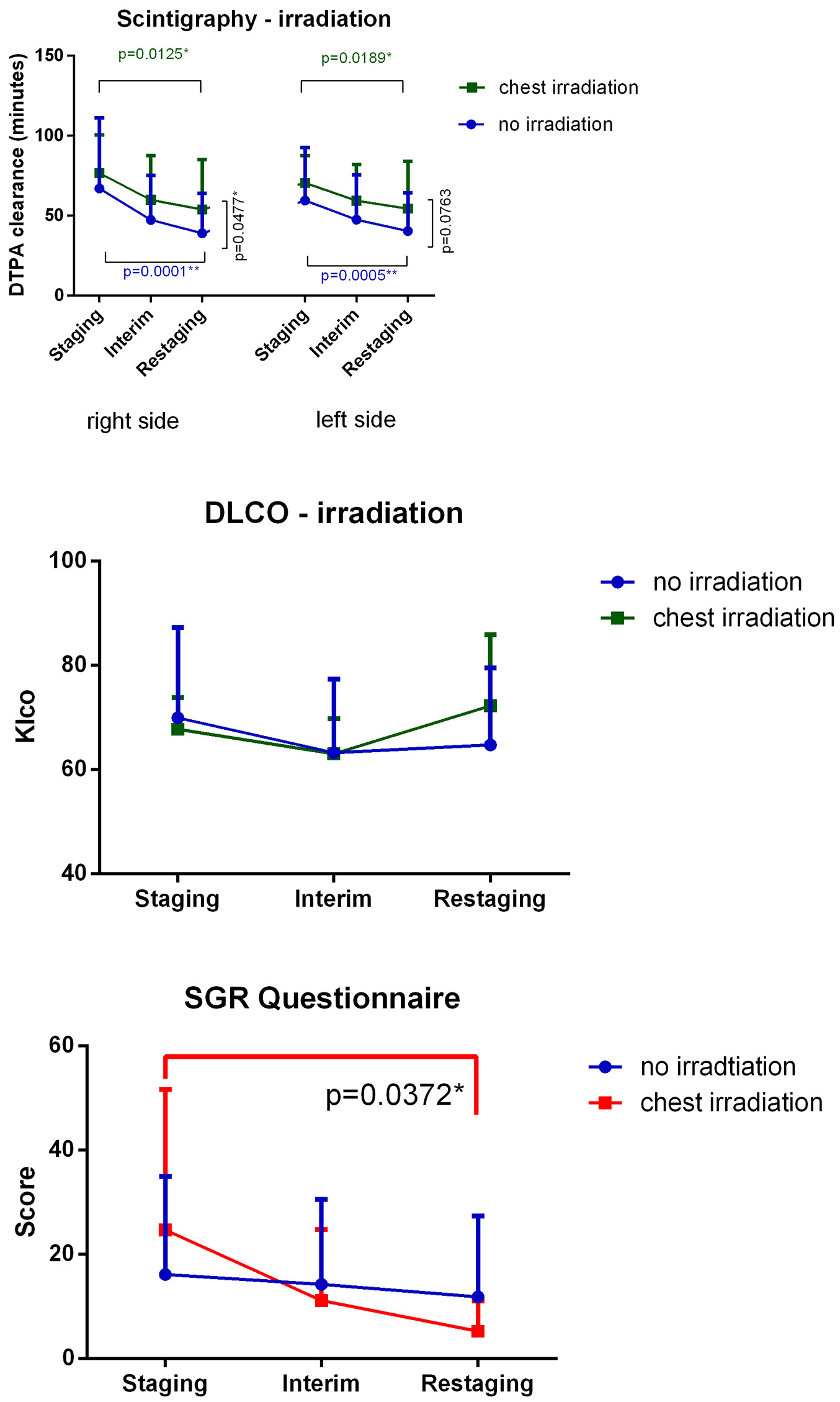
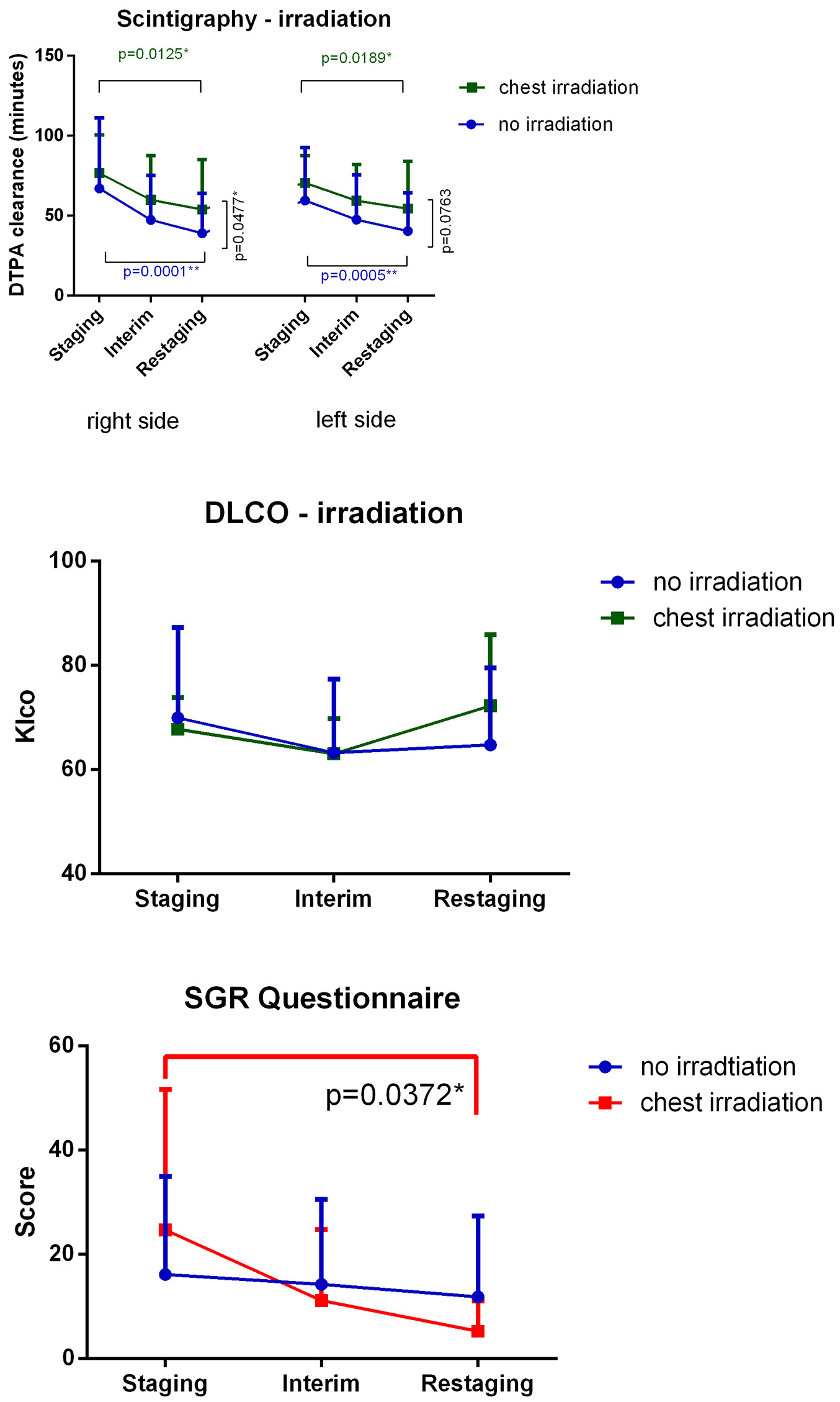
Figure 4. Mediastinal IFRT caused a significant degree of pulmonary toxicity. Findings evaluated via lung scintigraphy are shown. Changes observed in the no irradiation subgroup were greater than those observed in other groups. Changes in DLCO values were not significant. SGRQ scores decreased, and hence, subjective patient symptoms improved during treatment. Differences observed in the mediastinal irradiation group was significant. DTPA: diethylenetriamine pentaacetic acid; DLCO: carbon monoxide diffusion capacity of the lung; IFRT: involved-field irradiation therapy; Klco: transfer coefficient of the lung for carbon monoxide.
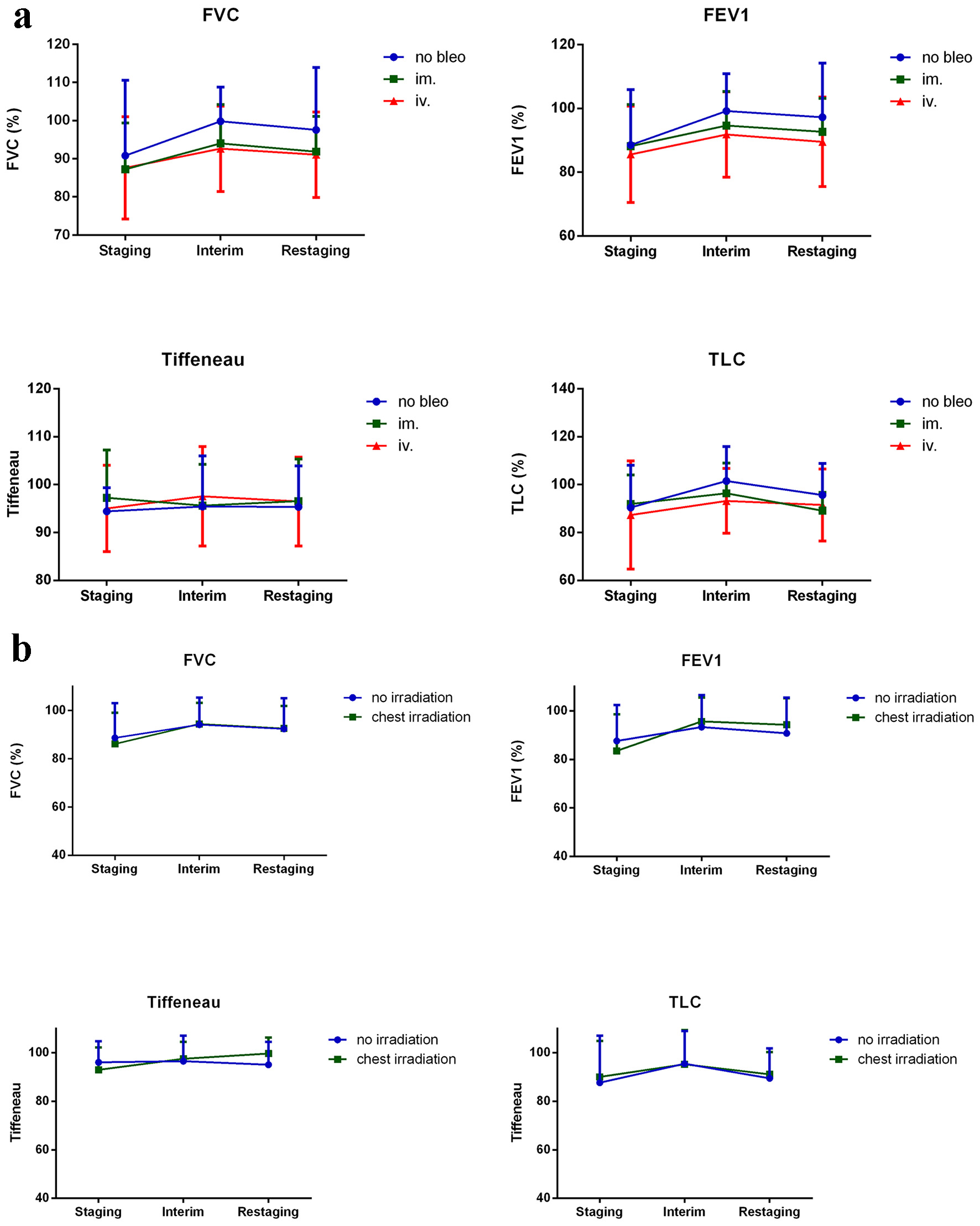
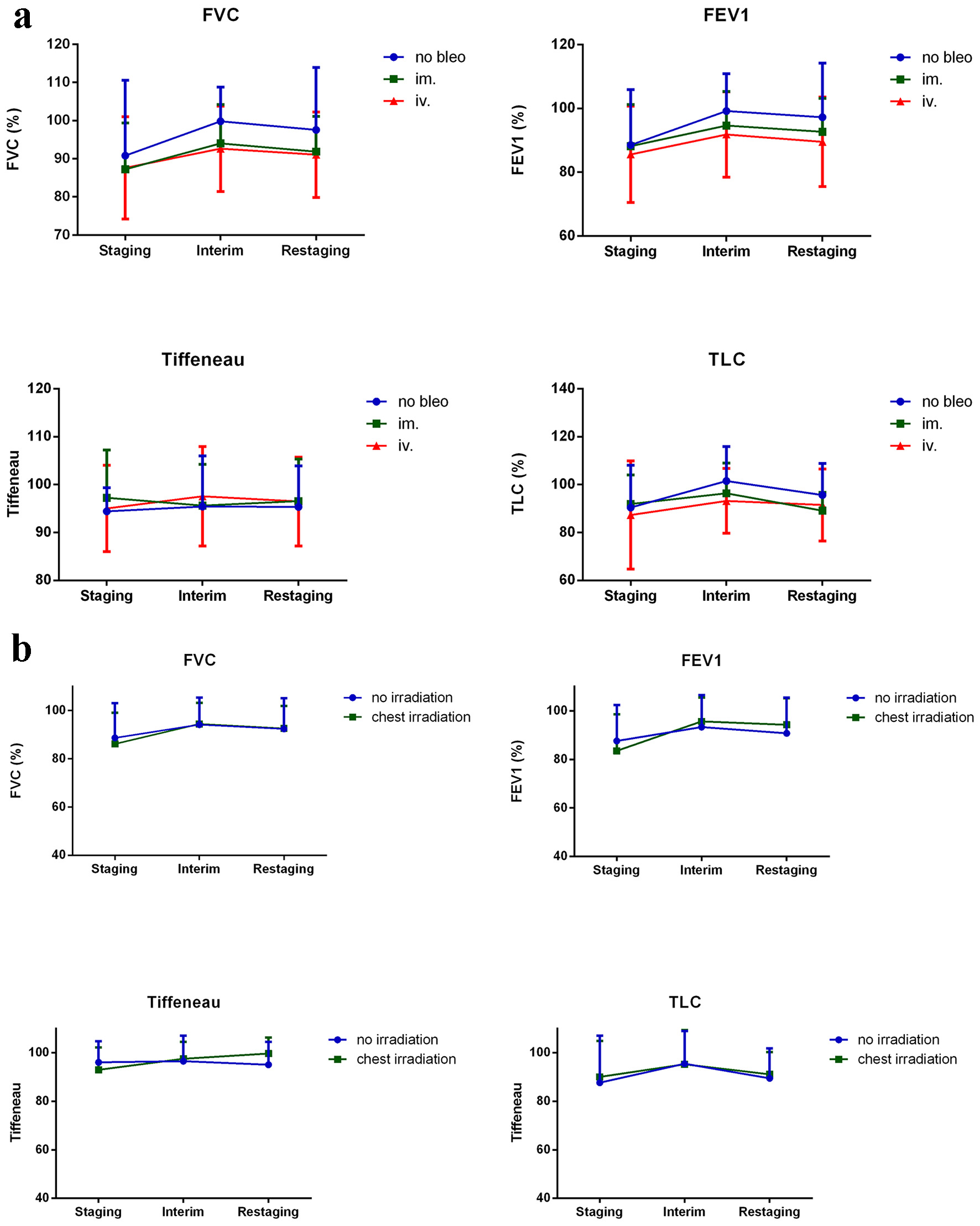
Figure 5. Spirometry results that did not significantly change during treatment are shown. (a) No differences in terms of bleomycin administration and (b) the presence or absence of mediastinal irradiation were observed. Results are shown as percentages of age-matched healthy controls. TLC: total lung capacity; FVC: forced vital capacity; FEV1: forced expiratory volume; Tiffeneau index: FEV1/vital capacity.
Table
Table 1. Patient Characteristics
| n (%) |
|---|
| Number of patients | 84 |
| Age (years, median, range) | 35 (18 - 80) |
| Male | 40 (47.6%) |
| Female | 44 (52.4%) |
| Male/female | 0.91 |
| B-symptoms | 44 (52.4%) |
| Histology | |
| cMC | 22 (26.2%) |
| cNS | 49 (58.3%) |
| cLR | 7 (8.3%) |
| cLD | 1 (1.2%) |
| ND | 5 (6.0%) |
| Stage | |
| I | 3 (3.6%) |
| II | 34 (40.5%) |
| III | 10 (11.9%) |
| IV | 37 (44.0%) |
| Treatment | |
| ABVD | 71 (84.5%) |
| BV-AVD | 12 (14.3%) |
| EVD | 1 (1.2%) |
| Mediastinal IFRT | 16 (19.0%) |
| Bleomycin administration | IM | IV | No bleomycin | P |
|---|
| cMC: classical mixed cellularity; cNS: classical nodular sclerosis; cLR: classical lymphocyte rich; cLD: classical lymphocyte depletion; ND: not determined; ABVD: doxorubicin, bleomycin, vinblastine, and dacarbazine; BV-AVD: brentuximab vedotin, doxorubicin, vinblastine, dacarbazine; EVD: epirubicin, vinblastine, dacarbazine; IFRT: involved-field irradiation therapy; IM: intramuscular; IV: intravenous; early/advanced: number and percentage of early stage and advanced stage patients; GFR: glomerular filtration rate; G-CSF: granulocyte colony-stimulating factor; ns: not significant. |
| n | 18 | 53 | 13 | |
| Age (years, median) | 33 (20 - 54) | 36 (18-75) | 35 (20-80) | ns |
| Early stage | 8 (44.4%) | 26 (49.1%) | 3 (23.1%) | ns |
| Advanced stage | 10 (55.6%) | 27 (50.9%) | 10 (76.9%) | |
| Bleomycin dose (mg/m2, median, range) | 120 (40 - 140) | 120 (40 - 120) | 0 | ns |
| Mediastinal IFRT | 9 (50%) | 5 (9.4%) | 2 (15.4%) | 0.0008 |
| Renal function (median GFR, mL/min/1.73 m2) | 90 | 90 | 90 | ns |
| Smoker | 8 (44.4%) | 15 (28.3%) | 7 (53.8%) | ns |
| G-CSF use | 8 (44.4%) | 31 (58.5%) | 12 (92.3%) | 0.0230 |
| Pulmonary involvement | 4 (22.2%) | 13 (24.5%) | 5 (38.5%) | ns |
| Bulky disease | 10 (55.6%) | 9 (17.0%) | 4 (30.8%) | 0.0063 |