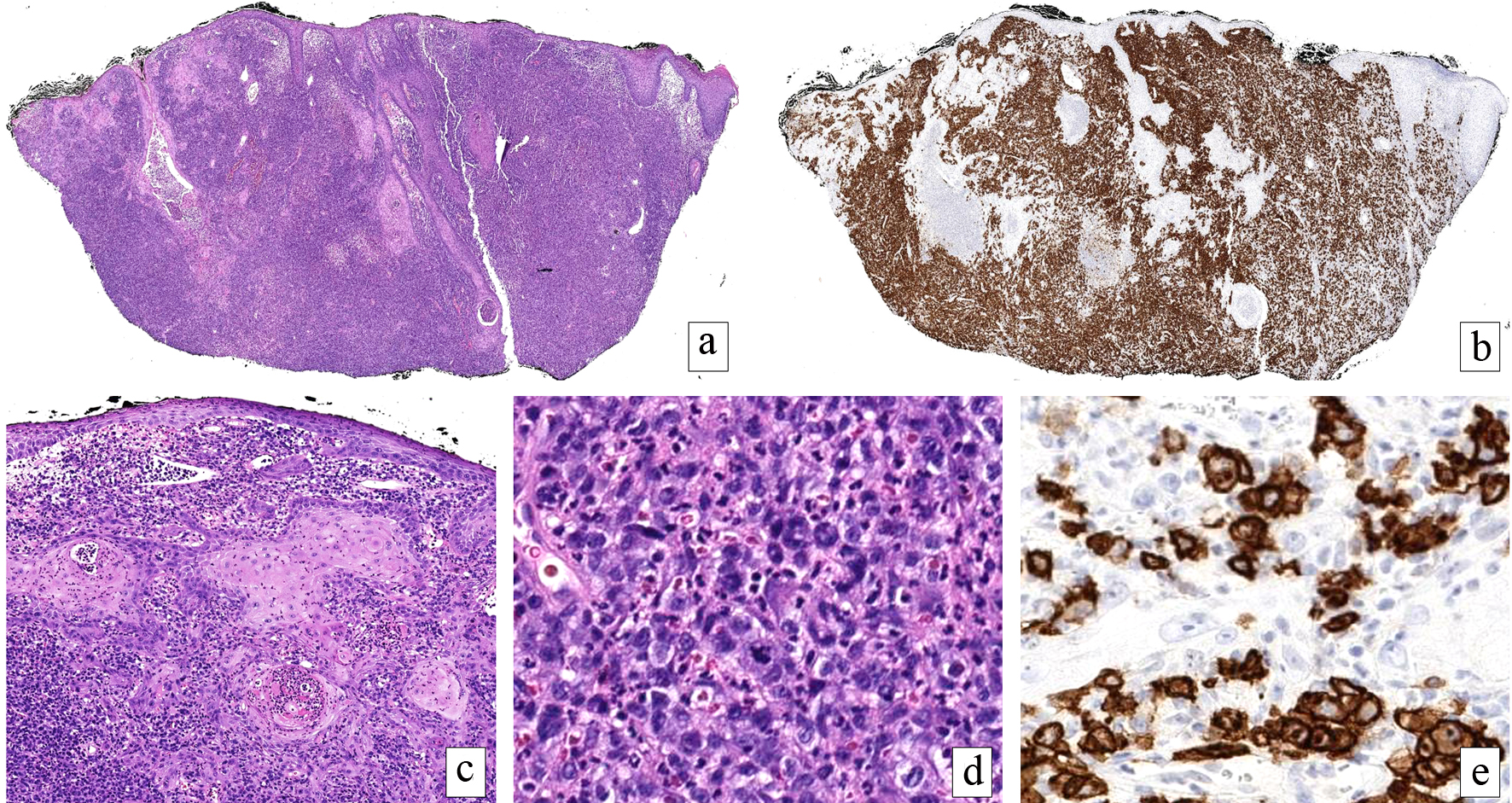
Figure 1. Primary cutaneous anaplastic large cell lymphoma. A dense, cellular infiltrate fills the dermis (H&E, × 20) (a) comprised of cells with uniform CD30 expression (× 20) (b). The overlying epidermis and follicular epithelium exhibit a reactive pseudoepitheliomatous hyperplasia mimicking squamous cell carcinoma (H&E, × 100) (c). Large, pleomorphic and mitotically active cells with bizarre nuclear contours predominate below the epidermal changes (H&E, × 200) (d). The markedly atypical cells exhibited an immunophenotype consistent with lymphoma. Higher power magnification of CD30 highlighting lesional cells (× 200) (e). The tumor cells were negative for ALK, CD20 and CD56, EBER, cytokeratin, 34BetaE12, and p63 (not shown). H&E: hematoxylin-eosin; ALK: anaplastic lymphoma kinase; EBER: Epstein-Barr virus-encoded small RNA.