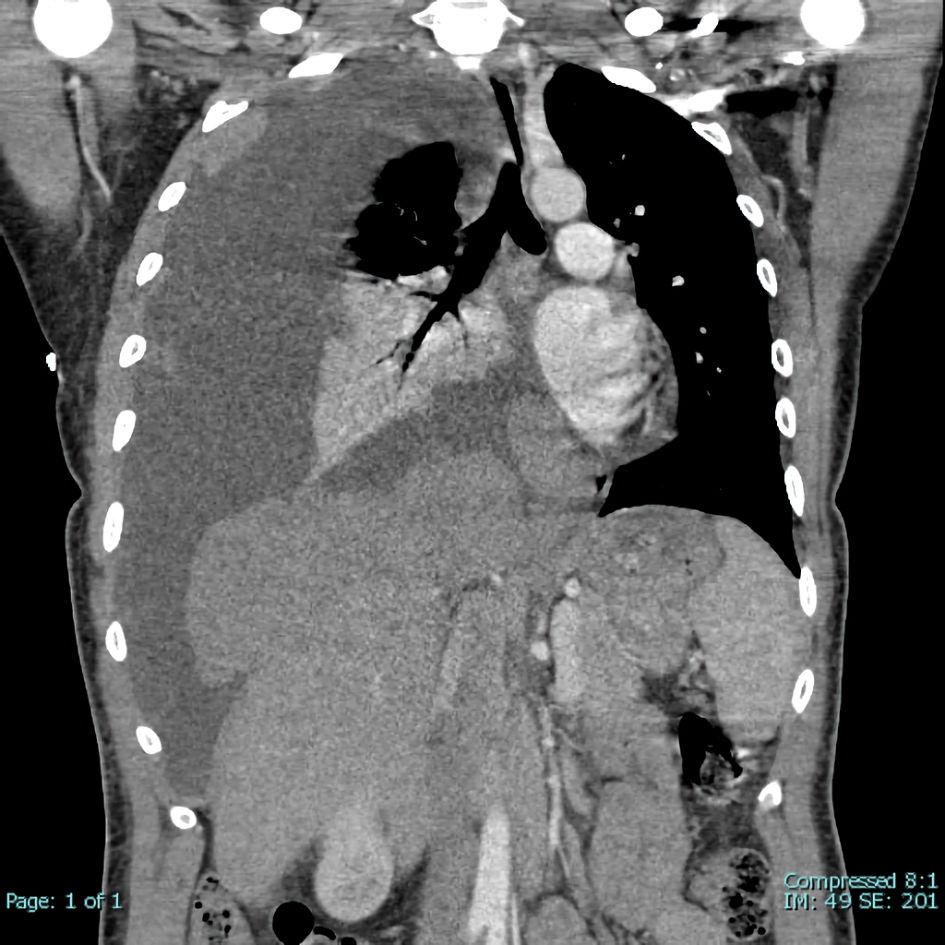
Figure 1. Extensive spread of right pleural-based soft tissue neoplasm. Very large right pleural effusion with secondary leftward mediastinal and tracheal shift. Partial collapse of right lung with air bronchograms.
| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website https://www.thejh.org |
Case Report
Volume 11, Number 6, December 2022, pages 223-232
Thymoma With Triple Threat: Pure Red Cell Aplasia, Autoimmune Hemolytic Anemia, and T-Cell Large Granular Lymphocytic Leukemia
Figures
Tables
| Labs | Result | Reference range |
|---|---|---|
| AIHA: autoimmune hemolytic anemia; PRCA: pure red cell aplasia; WBC: white blood cell; RBC: red blood cell; MCV: mean corpuscular volume; Ig Ser QN: quantitative serum immunoglobulins; Ig: immunoglobulin. | ||
| WBC count (× 103/µL) | 6.7 | 3.6 - 10.6 |
| RBC count (× 106/µL) | 1.89 | 3.71 - 5.17 |
| Hemoglobin (g/dL) | 6.1 | 12.0 - 15.0 |
| Hematocrit (%) | 16.7 | 35.0 - 49.0 |
| MCV (fL) | 88.3 | 81.0 - 99.0 |
| Platelet count (× 103/µL) | 153 | 150 - 450 |
| Reticulocyte count (%) | < 0.1 | 0.5 - 2.5 |
| Absolute reticulocyte count (cells/µL) | 1.5 | 21.0 - 115.0 |
| Reticulocyte index | 0.02 | ≥ 2.0 adequate response |
| Haptoglobin (mg/dL) | < 6.0 | 30.0 - 200.0 |
| Total bilirubin (mg/dL) | 0.7 | 0.3 - 1.2 |
| Erythropoietin (mIU/mL) | 730.9 | 2.6 - 18.5 |
| Direct antiglobulin test IgG | Positive | |
| Direct antiglobulin test C3 | Positive | |
| Autoantibody | Warm | |
| Ig Ser QN (mg/dL) | ||
| IgG | 813 | 700 - 1,500 |
| IgM | 66 | 60 - 300 |
| IgA | 86 | 60 - 400 |
| Tetanus toxoid IgG (IU/mL) | 2.02 | Immune if ≥ 0.01 IU/mL |
| Diphtheria toxoid IgG (IU/mL) | 0.02 | Immune if ≥ 0.01 IU/mL |
| References | Zaucha et al, 2007 [10] | Larroche et al, 2000 [11] | Palmieri et al, 1997 [9] |
|---|---|---|---|
| PO: per os; PRCA: pure red cell aplasia; IVIG: intravenous immunoglobulin; BID: twice a day; TID: three times a day; WHO: World Health Organization. aCorticosteroids combined with octreotide were contraindicated due to high risk of gastrointestinal bleeding. | |||
| Age | 35 | 75 | 56 |
| Sex | Female | Male | Female |
| Time between diagnoses | 4 - 6 months | Concurrent | 2 - 3 months |
| Hemoglobin at presentation (g/dL) | 8.2 | 2.8 | 5.8 |
| Reticulocyte count at presentation (%) | Information not available | 0 | Information not available |
| Transfusion dependence; frequency | Yes, frequency: 2 - 3 weeks | Yes, frequency: 1 week | Yes, frequency not specified |
| WHO histology | B1/B2 | B1/B2 | B1/B2 |
| Masaoka Koga staging | IVB | I | IIIB |
| Thymectomy | No | Yes | No |
| Response to thymectomy | Thymectomy not performed | Remained transfusion-dependent | Thymectomy not performed |
| Chemotherapy | Doxorubicin, cisplatin, cyclophosphamide, vincristine (6 cycles) | None | Cisplatin, prednisone, cyclophosphamide (6 cycles) |
| Cisplatin and etoposide (3 cycles) | |||
| Ifosfamide (6 cycles) | |||
| Other treatments | Recombinant human erythropoietin, duration: 4 months | Prednisone PO 1 mg/kg/day, duration: 1 month | Prednisone PO 1 mg/kg/day, duration: 1 month |
| Octreotide 20 mg IM q28d, duration: 3 monthsa | Octreotide 0.5 mg, subcutaneous TID + prednisone PO 0.7 mg/kg/day, duration: 1 month | Octreotide 0.5 mg subcutaneous TID + prednisone PO 0.6 mg/kg/day, duration: not specified | |
| IVIG 0.4 g/kg/day, duration: 5 days | |||
| Outcomes | No response to any round of chemotherapy | No response to single agent prednisone. Reticulocyte count 0%. | No response to any round of chemotherapy. |
| No response to prednisone with octreotide. Reticulocyte count 0% and patient remained transfusion-dependent. | With single agent prednisone, hemoglobin increased from 5.8 to 7.8 g/dL but patient remained transfusion-dependent. | ||
| No response to erythropoietin | |||
| After 3 months of octreotide, hemoglobin normalized, and bone marrow biopsy showed erythroid reconstitution. | 3 weeks after treatment with IVIG, hemoglobin increased from 7.0 to 10.8 g/dL. Reticulocyte count 2.0% and patient no longer required transfusions. | After 1 month of octreotide with prednisone, hemoglobin increased, and patient no longer required transfusions. After 15 months, patient was in complete remission with no evidence of thymoma on imaging. | |
| Patient remains in complete remission 1 year later. | |||
| Patient remains in complete remission > 21 months later. | Patient remains in complete remission > 3 years later. Continues to receive octreotide (0.5 mg BID) and prednisone (0.2 mg/kg/day). | ||
| References | Current case | Wang et al, 2020 [26], case 1 | Wang et al, 2020 [26], case 2 | Wang et al, 2020 [26], case 3 | Wang et al, 2020 [26], case 4 |
|---|---|---|---|---|---|
| RBC: red blood cell; WBC: white blood cell; PRCA: pure red cell aplasia; AIHA: autoimmune hemolytic anemia. WHO: World Health Organization. aResearchers did not specify whether corticosteroids or any other treatments were given. | |||||
| Timing | Concurrent | Concurrent | Concurrent | Concurrent | Concurrent |
| Age at diagnosis of thymoma (years) | 41 | 65 | 38 | 45 | 53 |
| Sex | Female | Female | Male | Male | Female |
| Hemoglobin pre-thymectomy (g/dL) | 6.1 | 3.9 | 7.3 | 6.5 | 8.5 |
| Reticulocyte count pre-thymectomy (%) | < 0.1 | 0.2 | 0.4 | 0.3 | 0.4 |
| RBC count pre-thymectomy (× 106/µL) | 1.89 | 1.07 | 2.34 | Information not available | Information not available |
| Total bilirubin; indirect bilirubin (mg/dL) | 0.4; information not available | 1.6; 1.2 | 1.5; 1.0 | 1.5; 1.0 | 0.8; 0.5 |
| Erythropoietin (mIU/mL) | 731 | > 797 | 630 | Information not available | Information not available |
| Lactate dehydrogenase (U/L) | Information not available | 293 | 290 | Information not available | Information not available |
| IgG direct antiglobulin test | + | + | + | + | + |
| C3 direct antiglobulin test | + | + | + | + | + |
| WHO histology | B2 | B2 + B3 | AB | AB | B2 |
| Masoaka Koga staging | IVA | III | I | IIA | I |
| Thymectomy | Yes (delayed) | Yes | Yes | Yes | Yes |
| Treatments | Corticosteroids, octreotide | Corticosteroids (without improvement) followed by thymectomy | Thymectomy only | Thymectomy onlya | Thymectomy onlya |
| Outcomes | Normalization of hemoglobin | Normalization of hemoglobin post-thymectomy | Normalization of hemoglobin post-thymectomy | Normalization of hemoglobin post-thymectomy | Normalization of hemoglobin post-thymectomy |
| Diagnosis | Treatment | Outcome |
|---|---|---|
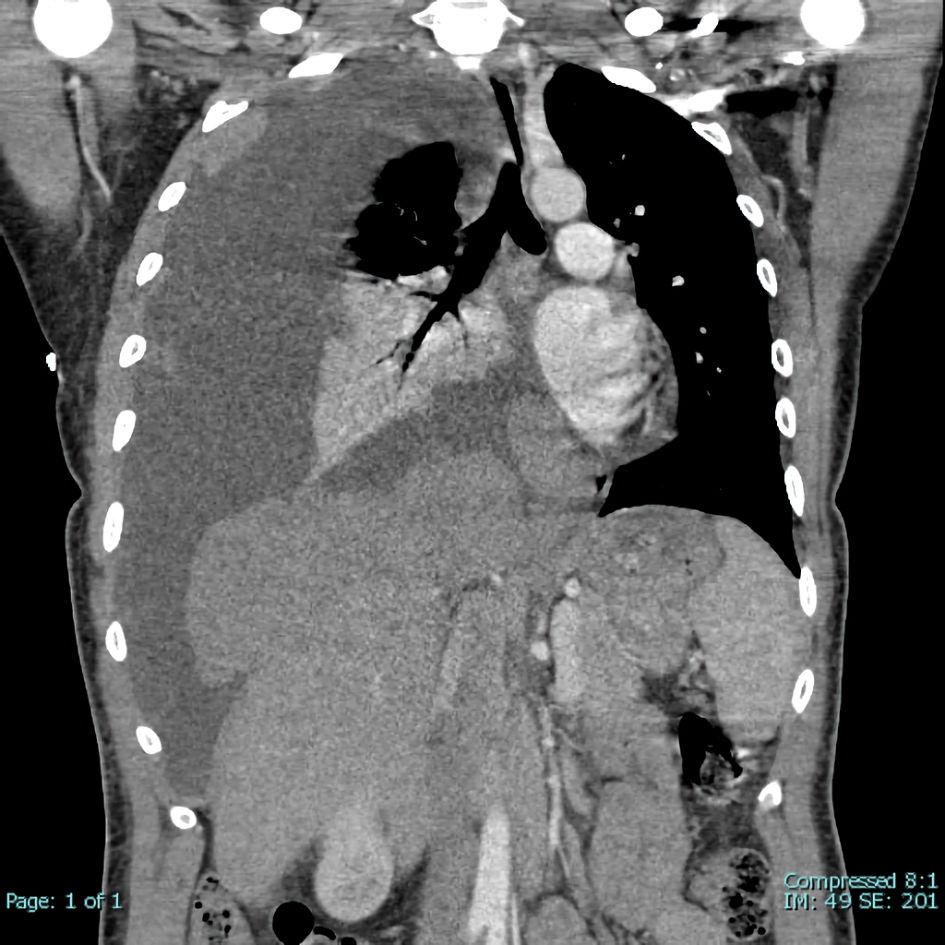
| Thymoma | Cisplatin, doxorubicin, cyclophosphamide | Stable disease for approximately 35 months, progression required thymectomy |
| Pure red cell aplasia | Octreotide and methylprednisolone | Partial remission |
| Autoimmune hemolytic anemia | Octreotide and methylprednisolone | Remission |
| Neutropenia, presumed autoimmune in origin | Anti-thymocyte globulin, tacrolimus, methylprednisolone, granulocyte colony stimulating factor, Intravenous immunoglobulin | Partial remission |
| T-cell large granular lymphocytic leukemia | Methotrexate | Remission |