| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Case Report
Volume 2, Number 2, October 2013, pages 79-84
Extensive Portal and Superior Mesenteric Vein Thrombosis After Splenectomy in a Patient With Hereditary Spherocytosis
Beatriz Lopesa, h, Ligia Almeidab, Alana Vicentec, Daniel Marcellosd, Marcelo Corassae, Fabio Freiref, Denis Szejnfeldg
aInternal Medicine at Universidade Federal de Sao Paulo (UNIFESP), Lopes, Rua Pedro de Toledo, 1069, ap 21. Vila Clementino. Sao Paulo-SP, Brazil
bInternal Medicine at Universidade Federal de Sao Paulo (UNIFESP), Rua Paraguacu, 479, ap 181. Perdizes. Sao Paulo-SP, Brazil
cInternal Medicine at Universidade Federal de Sao Paulo (UNIFESP), Rua Tagua, 261, ap 34. Liberdade. Sao Paulo-SP, Brazil
dInternal Medicine at Universidade Federal de Sao Paulo (UNIFESP), Rua Jose de Magalhaes, 373, ap 304. Vila Clementino. Sao Paulo-SP, Brazil
eInternal Medicine at Universidade Federal de Sao Paulo (UNIFESP), Rua Borges Lagoa, 1209, ap 2501. Vila Clementino. Sao Paulo-SP, Brazil
fInternal Medicine Department at Universidade Federal de Sao Paulo (UNIFESP), Rua Borges Lagoa, 908, ap 113. Vila Clementino. Sao Paulo-SP, Brazil
gInterventional Radiology at Universidade Federal de Sao Paulo (UNIFESP), Rua Detroit, 61, Brooklin. Sao Paulo-SP, Brazil
hCorresponding author: Beatriz Lopes, Rua Pedro de Toledo, 1069, ap 21. Vila Clementino. Sao Paulo-SP. Brazil
Manuscript accepted for publication August 15, 2013
Short title: Portal and Superior Mesenteric Vein Thrombosis
doi: https://doi.org/10.4021/jh84w
| Abstract | ▴Top |
Portal and superior mesenteric vein thrombosis are uncommon outcomes post-splenectomy. We reported the case of a patient with hereditary spherocytosis who evolved after splenectomy with extensive thrombosis of these veins and was treated with systemic anticoagulation and endovascular thrombolysis, a promising alternative.
Keywords: Splenectomy; Hereditary spherocytosis; Portal vein thrombosis; Mesenteric vein thrombosis; Interventional radiology
| Introduction | ▴Top |
Portal and superior mesenteric vein thrombosis are serious complications [1, 2]. The estimated incidence varies from 1.6% to 11% [3] and these values may be underestimated once many cases are asymptomatic and when symptoms exist they are nonspecific [4]. Clinical presentation may vary from mesenteric ischemia with necrosis to abdominal pain, nausea, vomiting, anorexia, fever, diarrhea and blood in stool. These symptoms are much more severe when superior mesenteric vein (SMV) is involved than only portal vein (PV) [2, 5-7].
Hereditary spherocytosis (HS) is a congenital hemolytic anemia with an incidence of about one in 2,000 - 5,000 people [8]. Splenectomy is recommended in some cases for symptoms control. However, it is known that spleen removal favors not only the classic susceptibility to encapsulated bacteria infections, but also increases long-term risk of arterial and venous thrombotic events [8-12].
There is still no consensus on the best approach to PV-SMV thrombosis after splenectomy. Perioperative prophylaxis with anticoagulation/antiplatelet therapy and treatment are controversial areas [7, 13-15]. However, at one point all agree: therapy should be instituted as soon as possible to avoid fatal complications [7, 16]. Systemic anticoagulation and thrombolytic therapy have low efficacy in extensive thrombosis of these sites [2]. Surgical treatment is indicated for those that evolve with intestinal necrosis. Recently, endovascular interventional techniques have been recognized as promising alternatives for PV-SMV treatment with good results so far [17, 18].
We will describe the case of a patient with HS who evolved in the post-operative of a splenectomy with extensive PV-SMV thrombosis and was treated with systemic anticoagulation and endovascular thrombolysis via superior mesenteric artery. This case report aims to review the main ways of clinical and interventional treatment for extensive portal-mesenteric thrombosis.
| Case Report | ▴Top |
A 20-year-old woman diagnosed with HS underwent splenectomy through open surgery with no complications and was discharged on the fourth day after procedure without having received anticoagulant therapy perioperatively. Prior to splenectomy, splenic index was 1,580 (normal: up to 480). From the fourth day after surgery she presented with progressive thrombocytosis (the highest value observed was 1.468 × 1012/L platelets on the 21st day). Intense abdominal pain in right upper quadrant associated with nausea, vomiting and diarrhea was referred in the 9th day. In abdominal ultrasonography it was observed an increased PV diameter (1.5 cm) with echogenic material inside and no flow at color and spectral Doppler, compatible with PV thrombosis.
Promptly, low molecular weight heparin (enoxaparin 60 mg each 12 hours), warfarin and analgesia were introduced. Diagnostic approach continued with a computed tomography (CT) angiography that demonstrated extensive SMV, splenic vein, PV and intrahepatic left branch thrombosis (Fig. 1, 2). Given the extensive thrombosis and considering that SMV was involved, medical team decided to carry out intra-arterial thrombolysis. The procedure was performed through the femoral artery followed by mesenteric arteriography which demonstrated slowed venous phase with no opacification of SMV and PV. Periportal collateral circulation was exuberant (Fig. 3). A alteplase bollus with 10mg intra-arterial was done followed by maintenance infusion rate of 1 mg/h. Concomitantly, systemic continuous infusion with unfractionated heparin was started in order to maintain APTT between 2.0 and 2.5 times control. Twenty four hours after the beginning of thrombolysis, CT angiography was performed and it still showed extensive mesenteric and splenic veins thrombosis surrounded by a large amount of collateral veins with only partial recanalization of intrahepatic branches (Fig. 4). Assistant team decided to keep the infusion catheter but in a rate of 2 mg/h. After 24 hours, another CT angiography was done and no significant change was observed. At that moment, thrombolytic infusion was discontinued due to potential cumulative risk of bleeding and progressive clinical improvement. There were no complications during procedure and the patient remained asymptomatic. Before discharge, an upper digestive endoscopy was performed and there were no evidence of esophageal varices or hypertensive gastropathy. Patient was discharged taking warfarin for outpatient hematology follow up.
 Click for large image | Figure 1. CT angiography with extensive SMV, splenic vein, PV and intrahepatic left branch thrombosis. |
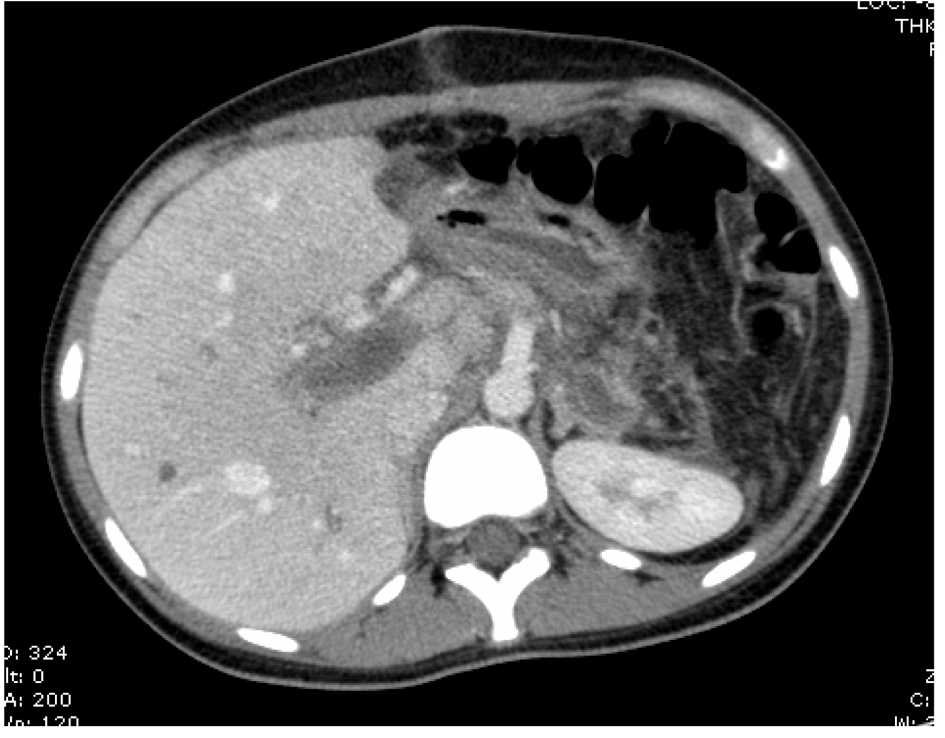 Click for large image | Figure 2. Axial CT abdome angiography with extensive portal vein thombus. |
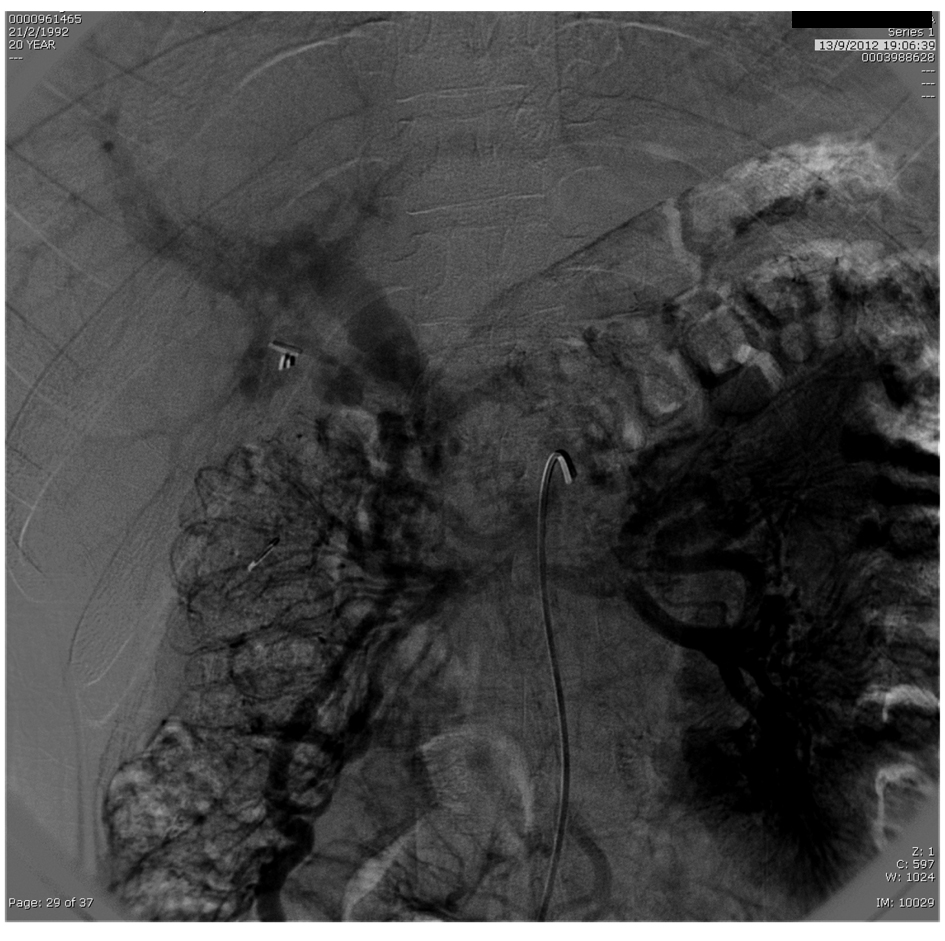 Click for large image | Figure 3. Mesenteric arteriography with slowed venous phase with no opacification of SMV and PV. Exuberant periportal collateral circulation. |
 Click for large image | Figure 4. CT angiography with extensive mesenteric and splenic veins thrombosis surrounded by a large amount of collateral veins with only partial recanalization of intrahepatic branches. |
| Discussion | ▴Top |
PV-SMV thrombosis usually presents with nonspecific symptoms such as abdominal pain, nausea, vomiting, anorexia, fever, diarrhea and blood in stool, which makes diagnosis difficult in many cases. However, it can also lead to severe complications with high mortality (5% to 37%) such as intestinal ischemia, necrosis, perforation, peritonitis and, lately, variceal bleeding due to portal hypertension [2, 5-7]. Onset of symptoms is variable in series of cases and may appear 2 - 42 days after surgery [4, 19, 20]. In this case, abdominal pain, nausea, vomiting and diarrhea appeared nine days after surgical procedure.
Contributing factors for thrombosis after splenectomy are the underlying disease, spleen size, postoperative thrombocytosis and a hypercoagulable state provided by the organ removal [21]. Splenomegaly is accompanied by an increased splenic vein diameter and, consequently, when spleen is removed, blood flow slows down in this vessel, which contributes to thrombus formation [19]. It is also believed that splenectomy favors a hyperviscosity state due to thrombocytosis and postoperative leukocytosis since there is no splenic lysis of these cells [22]. Moreover, it is observed a stiffness in red blood cells due to Howell-Jolly corpuscles which also contributes to enhanced plasma viscosity favoring thrombosis [23].
The direct association of thrombocytosis after splenectomy and PV-SMV thrombosis is still not very clear but platelets raise should be considered an important risk factor [21]. In a large study with 147 patients who underwent splenectomy there was a direct association between platelet count above 0.65 × 1012/L and development of portal system thrombosis. Because of this, authors recommended administration of antiplatelet agents after splenectomy to all patients presenting severe thrombocytosis [13].
Despite all these risk factors, anticoagulant prophylaxis for thrombosis after splenectomy is still a controversial point. European Association for Endoscopic Surgery recommends prophylactic anticoagulation with subcutaneous heparin during perioperative period for all patients who underwent splenectomy and it should be maintained for four weeks in those at high risk of thrombosis [24]. High risk patients are those who present hypercoagulopathy, hemolytic anemia, hypersplenism, hematologic malignancy and splenomegaly [25].
Splenectomy is indicated in some cases of HS for symptoms control but it is already known that spleen removal can cause a lot of complications [8-12]. Not only thrombocytosis but the raising in hematocrit and decreasing in bilirubin levels are implicated in increased risk of thrombosis post-splenectomy in those with hemolytic anemia [26]. The Framingham study demonstrated that patients with high hematocrit levels have two-fold increased risk of stroke compared to those with low values [27]. Several studies have shown that mild to moderate elevation in bilirubin levels are associated with lower risk of atherosclerosis due to a possible antioxidant property [28-30]. Thrombocytosis post-splenectomy tends to be transient. However, patients with HS usually persist with high platelet levels for long periods increasing risk of thrombosis [8]. Thus, in those with mild to moderate anemia the benefit of splenectomy should be carefully analyzed because of substantial risk of vascular events [8].
Our patient had not only hemolytic anemia, but also splenomegaly, postoperative thrombocytosis reaching more than 1 × 1012/L and no anticoagulant prophylaxis was prescribed. All of this possibly contributed to the extent of thrombosis in the case.
There is no guideline for treatment of PV-SMV thrombosis post splenectomy. However, all agree that therapy should be instituted as soon as possible to avoid fatal complications [7, 16]. Traditionally, it is described the clinical treatment with systemic anticoagulation or thrombolysis and the surgical approach. Surgical intervention should be done in cases of tissue injury: ischemia and/or intestinal necrosis [13]. Some studies have shown that early oral anticoagulation promotes recanalization in approximately 35% of cases [31, 32]. However, anticoagulation success is much less likely when there is extensive thrombosis once it is a therapy of low effectiveness [2, 33].
Recently, endovascular interventional techniques have been recognized as promising alternatives for PV-SMV thrombosis treatment with good results so far [17, 18]. There are two types of interventions: thrombolytic infusion in situ and mechanical thrombectomy [34]. Thrombolytic therapy can be administered directly into the portal vein via transjugular intrahepatic [35-37] or percutaneous transhepatic pathways [38-40] or indirectly via superior mesenteric artery by femoral or radial artery catheterization [41-43]. Better results were demonstrated with direct techniques [44]. The direct infusion into the PV-SMV greatly increases thrombolytic effect, reduces the required drug dose and, thereby, diminishes bleeding risk [44]. Indirect thrombolysis is technically simpler and enables thrombolytic to be infused in small mesenteric venous branches [42, 43]. However, it does not enable direct contact of the agent and thrombus requiring a longer infusion period and, therefore, increasing risk of bleeding complications [35]. Combination of mechanical thrombectomy with direct thrombolysis proved to be more effective compared with only directly or indirectly thrombolytic therapy [35, 45, 46].
In this case we proceeded indirect thrombolysis via superior mesenteric artery aiming to enable thrombolytic agent to spread through the small mesenteric venous branches all occluded by thrombi. Despite the increased risk of bleeding described with this technique [35], there was no bleeding complication. Alteplase was used for thrombolysis and unfractionated systemic heparin was introduced concomitantly because fibrinolysis provides a pro-thrombotic state increasing risk of new thrombus formation and propagation of the already established ones [44].
There was no immediate recanalization of PV-SMV despite early onset of systemic anticoagulation and subsequent endovascular thrombolytic therapy. Several factors may have contributed to this outcome but perhaps the most important one was the fact that thrombolytic therapy was introduced only 10 days after symptoms onset. When alteplase was initiated the patient was already less symptomatic, probably due to collateral veins formation. Possibly, recanalization would have been reached with an earlier introduction of endovascular therapy. In a case series of six patients diagnosed with extensive post-splenectomy PV-SMV thrombosis, systemic anticoagulation was initiated promptly and after an average of 3.5 days in situ thrombolysis was introduced due to persistent symptoms. Four of these patients had complete recanalization and residual thrombosis was observed in only 20% [34].
Direct techniques of thrombolysis proved to be more effective than indirect ones [44] and association of thrombolytic with mechanical thrombectomy showed a higher success rate than the use of intravascular medication only [35, 45, 46]. Thus, a satisfactory result could have been achieved if a direct technique associated with thrombectomy had been done. The infusion of alteplase was kept for two days and there are reports of up to 13 days of infusion without complications and with successful results [44].
Although recanalization did not occur immediately in this case, it is known that it could happens within four to six months of systemic anticoagulation.
There are still many controversial points about deep venous thrombosis not localized in the lower limbs. No consensus exists on prevention and treatment of thrombosis after splenectomy. However, as illustrated by this report, it seems reasonable to prescribe prophylaxis in these cases. Randomized controlled studies are desirable in order to help elucidating the best therapeutic option for this patient profile.
Grant Support
None.
Financial Disclosures
None.
| References | ▴Top |
- Sobhonslidsuk A, Reddy KR. Portal vein thrombosis: a concise review. Am J Gastroenterol. 2002;97(3):535-541.
doi pubmed - Kumar S, Sarr MG, Kamath PS. Mesenteric venous thrombosis. N Engl J Med. 2001;345(23):1683-1688.
doi pubmed - Brink JS, Brown AK, Palmer BA, Moir C, Rodeberg DR. Portal vein thrombosis after laparoscopy-assisted splenectomy and cholecystectomy. J Pediatr Surg. 2003;38(4):644-647.
doi pubmed - Chaffanjon PC, Brichon PY, Ranchoup Y, Gressin R, Sotto JJ. Portal vein thrombosis following splenectomy for hematologic disease: prospective study with Doppler color flow imaging. World J Surg. 1998;22(10):1082-1086.
doi pubmed - Llado L, Fabregat J, Castellote J, Ramos E, Torras J, Jorba R, Garcia-Borobia F, et al. Management of portal vein thrombosis in liver transplantation: influence on morbidity and mortality. Clin Transplant. 2007;21(6):716-721.
pubmed - Shibahara K, Tatsuta K, Orita H, Yonemura T, Kohno H. Superior mesenteric and portal vein thrombosis caused by congenital antithrombin III deficiency: report of a case. Surg Today. 2007;37(4):308-310.
doi pubmed - Soyer T, Ciftci AO, Tanyel FC, Senocak ME, Buyukpamukcu N. Portal vein thrombosis after splenectomy in pediatric hematologic disease: risk factors, clinical features, and outcome. J Pediatr Surg. 2006;41(11):1899-1902.
doi pubmed - Troendle SB, Adix L, Crary SE, Buchanan GR. Laboratory markers of thrombosis risk in children with hereditary spherocytosis. Pediatr Blood Cancer. 2007;49(6):781-785.
doi pubmed - Schilling RF. Spherocytosis, splenectomy, strokes, and heat attacks. Lancet. 1997;350(9092):1677-1678.
doi - Hoeper MM, Niedermeyer J, Hoffmeyer F, Flemming P, Fabel H. Pulmonary hypertension after splenectomy? Ann Intern Med. 1999;130(6):506-509.
doi pubmed - Jardine DL, Laing AD. Delayed pulmonary hypertension following splenectomy for congenital spherocytosis. Intern Med J. 2004;34(4):214-216.
doi pubmed - Hayag-Barin JE, Smith RE, Tucker FC, Jr. Hereditary spherocytosis, thrombocytosis, and chronic pulmonary emboli: a case report and review of the literature. Am J Hematol. 1998;57(1):82-84.
doi - Stamou KM, Toutouzas KG, Kekis PB, Nakos S, Gafou A, Manouras A, Krespis E, et al. Prospective study of the incidence and risk factors of postsplenectomy thrombosis of the portal, mesenteric, and splenic veins. Arch Surg. 2006;141(7):663-669.
doi pubmed - Fujita F, Lyass S, Otsuka K, Giordano L, Rosenbaum DL, Khalili TM, Phillips EH. Portal vein thrombosis following splenectomy: identification of risk factors. Am Surg. 2003;69(11):951-956.
pubmed - Rossi E, Michelini ME, Pignatti CB, Zanotti F, Franchella A. A case of portal vein thrombosis after laparoscopy-assisted splenectomy and cholecystectomy in a child. J Pediatr Surg. 2007;42(8):1449-1451.
doi pubmed - Ikeda M, Sekimoto M, Takiguchi S, Kubota M, Ikenaga M, Yamamoto H, Fujiwara Y, et al. High incidence of thrombosis of the portal venous system after laparoscopic splenectomy: a prospective study with contrast-enhanced CT scan. Ann Surg. 2005;241(2):208-216.
doi pubmed - Streitparth F, Santosa F, Milz J, Gebauer B, Teichgraber U, Hamm B, Hidajat N. [Transjugular intrahepatic portosystemic shunt in patients with portal vein thrombosis]. Rofo. 2008;180(10):899-905.
pubmed - Li CQ, Mao Y, Xu DH, Zhou A, Li P. Clinical observation on interventional recanalization of portal vein stenosis and occlusion due to thrombosis. Zhongguo Gandan Waike Zazhi 2007; 13:304-306.
- Rattner DW, Ellman L, Warshaw AL. Portal vein thrombosis after elective splenectomy. An underappreciated, potentially lethal syndrome. Arch Surg. 1993;128(5):565-569; discussion 569-570.
doi pubmed - Broe PJ, Conley CL, Cameron JL. Thrombosis of the portal vein following splenectomy for myeloid metaplasia. Surg Gynecol Obstet. 1981;152(4):488-492.
pubmed - Winslow ER, Brunt LM, Drebin JA, Soper NJ, Klingensmith ME. Portal vein thrombosis after splenectomy. Am J Surg. 2002;184(6):631-635; discussion 635-636.
doi - Boxer MA, Braun J, Ellman L. Thromboembolic risk of postsplenectomy thrombocytosis. Arch Surg. 1978;113(7):808-809.
doi pubmed - Robertson DA, Simpson FG, Losowsky MS. Blood viscosity after splenectomy. Br Med J (Clin Res Ed). 1981;283(6291):573-575.
doi - Habermalz B, Sauerland S, Decker G, Delaitre B, Gigot JF, Leandros E, Lechner K, et al. Laparoscopic splenectomy: the clinical practice guidelines of the European Association for Endoscopic Surgery (EAES). Surg Endosc. 2008;22(4):821-848.
doi pubmed - Ikeda M, Sekimoto M, Takiguchi S, Yasui M, Danno K, Fujie Y, Kitani K, et al. Total splenic vein thrombosis after laparoscopic splenectomy: a possible candidate for treatment. Am J Surg. 2007;193(1):21-25.
doi pubmed - Schilling RF, Gangnon RE, Traver MI. Delayed adverse vascular events after splenectomy in hereditary spherocytosis. J Thromb Haemost. 2008;6(8):1289-1295.
doi pubmed - Kannel WB, Gordon T, Wolf PA, McNamara P. Hemoglobin and the risk of cerebral infarction: the Framingham Study. Stroke. 1972;3(4):409-420.
doi pubmed - Novotny L, Vitek L. Inverse relationship between serum bilirubin and atherosclerosis in men: a meta-analysis of published studies. Exp Biol Med (Maywood) 2003; 228:568-571.
- Vitek L, Novotny L, Sperl M, Holaj R, Spacil J. The inverse association of elevated serum bilirubin levels with subclinical carotid atherosclerosis. Cerebrovasc Dis. 2006;21(5-6):408-414.
doi pubmed - Sedlak TW, Snyder SH. Messenger molecules and cell death: therapeutic implications. JAMA. 2006;295(1):81-89.
doi pubmed - Turnes J, Garcia-Pagan JC, Gonzalez M, Aracil C, Calleja JL, Ripoll C, Abraldes JG, et al. Portal hypertension-related complications after acute portal vein thrombosis: impact of early anticoagulation. Clin Gastroenterol Hepatol. 2008;6(12):1412-1417.
doi pubmed - Condat B, Pessione F, Helene Denninger M, Hillaire S, Valla D. Recent portal or mesenteric venous thrombosis: increased recognition and frequent recanalization on anticoagulant therapy. Hepatology. 2000;32(3):466-470.
doi pubmed - Amitrano L, Guardascione MA, Scaglione M, Pezzullo L, Sangiuliano N, Armellino MF, Manguso F, et al. Prognostic factors in noncirrhotic patients with splanchnic vein thromboses. Am J Gastroenterol. 2007;102(11):2464-2470.
doi pubmed - Wang MQ, Lin HY, Guo LP, Liu FY, Duan F, Wang ZJ. Acute extensive portal and mesenteric venous thrombosis after splenectomy: treated by interventional thrombolysis with transjugular approach. World J Gastroenterol. 2009;15(24):3038-3045.
doi pubmed - Sze DY, O'Sullivan GJ, Johnson DL, Dake MD. Mesenteric and portal venous thrombosis treated by transjugular mechanical thrombolysis. AJR Am J Roentgenol. 2000;175(3):732-734.
doi pubmed - Aytekin C, Boyvat F, Kurt A, Yologlu Z, Coskun M. Catheter-directed thrombolysis with transjugular access in portal vein thrombosis secondary to pancreatitis. Eur J Radiol. 2001;39(2):80-82.
doi - Ferro C, Rossi UG, Bovio G, Dahamane M, Centanaro M. Transjugular intrahepatic portosystemic shunt, mechanical aspiration thrombectomy, and direct thrombolysis in the treatment of acute portal and superior mesenteric vein thrombosis. Cardiovasc Intervent Radiol. 2007;30(5):1070-1074.
doi pubmed - Hollingshead M, Burke CT, Mauro MA, Weeks SM, Dixon RG, Jaques PF. Transcatheter thrombolytic therapy for acute mesenteric and portal vein thrombosis. J Vasc Interv Radiol. 2005;16(5):651-661.
doi pubmed - Ozkan U, Oguzkurt L, Tercan F, Tokmak N. Percutaneous transhepatic thrombolysis in the treatment of acute portal venous thrombosis. Diagn Interv Radiol. 2006;12(2):105-107.
pubmed - Guglielmi A, Fior F, Halmos O, Veraldi GF, Rossaro L, Ruzzenente A, Cordiano C. Transhepatic fibrinolysis of mesenteric and portal vein thrombosis in a patient with ulcerative colitis: a case report. World J Gastroenterol. 2005;11(13):2035-2038.
pubmed - Wang MQ, Guo LP, Lin HY, Liu FY, Duan F, Wang ZJ. Transradial approach for transcatheter selective superior mesenteric artery urokinase infusion therapy in patients with acute extensive portal and superior mesenteric vein thrombosis. Cardiovasc Intervent Radiol. 2010;33(1):80-89.
doi pubmed - Antoch G, Taleb N, Hansen O, Stock W. Transarterial thrombolysis of portal and mesenteric vein thrombosis: a promising alternative to common therapy. Eur J Vasc Endovasc Surg. 2001;21(5):471-472.
doi pubmed - Safieddine N, Mamazza J, Common A, Prabhudesai V. Splenic and superior mesenteric artery thrombolytic infusion therapy for acute portal and mesenteric vein thrombosis. Can J Surg. 2007;50(1):68-69.
pubmed - Liu FY, Wang MQ, Fan QS, Duan F, Wang ZJ, Song P. Interventional treatment for symptomatic acute-subacute portal and superior mesenteric vein thrombosis. World J Gastroenterol. 2009;15(40):5028-5034.
doi pubmed - Lopera JE, Correa G, Brazzini A, Ustunsoz B, Patel S, Janchai A, Castaneda-Zuniga W. Percutaneous transhepatic treatment of symptomatic mesenteric venous thrombosis. J Vasc Surg. 2002;36(5):1058-1061.
doi pubmed - Kim HS, Patra A, Khan J, Arepally A, Streiff MB. Transhepatic catheter-directed thrombectomy and thrombolysis of acute superior mesenteric venous thrombosis. J Vasc Interv Radiol. 2005;16(12):1685-1691.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.