| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Original Article
Volume 2, Number 1, June 2013, pages 8-13
Correlation of Bone Marrow Aspirate, Biopsies and Touch Imprint Findings in Pancytopenia
Sudha Horakereppa Metikurkea, Krishnappa Rashmia, b, Rishi Bhavikaa
aDepartment of pathology, MS Ramaiah Medical Teaching College, India
bCorresponding author: Krishnappa Rashmi, 1st floor, 1st main, Kengeri satellite town, Bangalore, India
Manuscript accepted for publication May 27, 2013
Short title: Bone Marrow in Pancytopenia
doi: https://doi.org/10.4021/jh76w
| Abstract | ▴Top |
Background: Pancytopenia is the feature of many life threatening conditions. It is described as the deficiency of all three cellular elements of blood resulting in anemia, leucopenia and thrombocytopenia. It is a common hematological entity that we come across in routine practice. A comprehensive clinical, hematological and bone marrow study of patients usually helps in identification of the underlying cause. However in view of a wide array of etiological factors pancytopenia continues to be a challenge. Aspiration of the marrow is an indispensible adjunct to the study of hematopoietic disorders, if performed correctly. It is simple, safe and can be repeated. In case of trephine biopsy the greater value is that it can provide information about the structure of relatively large pieces of marrow. At the same time morphological features of individual cells may be identified by making imprint from the material obtained. Hence the present study was undertaken to evaluate the accuracy of the three components of marrow examination in the diagnosis of hematological disorders presenting with pancytopenia.
Methods: A total of 58 patients presenting with pancytopenia on initial workup requiring bone marrow aspirate and biopsy at MS Ramaiah medical college and hospital, Bangalore were studied from October 2009 to September 2011. Smears were made from the bone marrow aspirate (BMA), stained by Leishmann stain and examined. Touch imprints of bone marrow biopsy (BMB) were made and examined before the tissue was put in fixative (10% neutral buffered formalin) and subsequently processed, embedded in paraffin and sections were prepared and examined.
Results: Fifty eight patients with hematological diagnosis of pancytopenia were studied during the period October 2009 to September 2011. The sex distribution of pancytopenia showed male preponderance (60%). Most of the patients were in the age group of 21 - 30 years (25%) and least occurrence was seen in patients more than seventy years (3.45%). The commonest cause of pancytopenia was megaloblastic anemia (39.65%), followed by nutritional anemia (24.13%) and Aplastic anemia (12.06%). Eleven patients (18.9%) were diagnosed on bone marrow biopsy. Forty four out of the total fifty eight cases showed a positive correlation.
Conclusion: The commonest cause of pancytopenia was megaloblastic anemia. Clinical history and bone marrow examination is critical in arriving at the diagnosis. There was a positive correlation of 75.8% between BMA and BMB. Both the procedures were complimentary to each other and should be performed simultaneously along with imprint smears for complete bone marrow workup and evaluation.
Keywords: Pancytopenia; Bone marrow aspiration; Bone marrow biopsy; Megaloblastic anemia
| Introduction | ▴Top |
Sir William Harvey described blood as “the fountain of life and the primary seat of the soul. The marrow of our bones is the seedbed of our blood” [1], careful assessment of the blood elements is often the first step in assessment of hematological function and diagnosis.
The adult haematopoietic system includes tissues and organs involved in the proliferation, maturation and destruction of haematopoietic cells. These organs and tissues include the bone marrow, thymus, spleen and lymph nodes. Bone marrow is the site of myeloid, erythroid, and megakaryocytic as well as lymphoid cell development [2].
Examination of the marrow is critically important in the study and management of wide variety of haematological disorders. The spectrum of disorders primarily or secondarily affecting the bone marrow may manifest with peripheral pancytopenia [3].
Pancytopenia is the feature of many life threatening conditions. It is described as the deficiency of all three cellular elements of blood, resulting in anemia, leucopenia and thrombocytopenia [4].
The complete hematological workup with good clinical correlation is of utmost importance to evaluate the cause of pancytopenia as its treatment is dictated by the nature of underlying disease. Aspiration of the bone marrow is an indispensable adjunct to the study of haematopoietic disorders, if performed correctly, it is simple, safe and can be repeated.
In case of trephine biopsy the greater value is that it can provide information about the structure of relatively large pieces of marrow. At the same time morphological features of individual cells may be identified by making an imprint from the material obtained [5].
Objectives
1), to correlate the findings of bone marrow aspirate, bone marrow biopsy and touch imprints in the diagnosis of pancytopenia; 2), to study the various conditions presenting with pancytopenia requiring bone marrow examination.
| Materials and Methods | ▴Top |
Patients presenting with pancytopenia on initial work up requiring bone marrow aspirate and bone marrow biopsy at M.S. Ramaiah Medical College from October 2009 to September 2011 are included in this study. Patients with pancytopenia secondary to drugs, chemotherapy and radiotherapy were excluded from the study.
Criteria for the diagnosis of pancytopenia are hemoglobin less than 10 g/dL, TLC less than 4 × 103/µL and platelet count less than 1.0 × 103/µL. The peripheral smear was studied after staining with Leishmann stain. Subsequently a bone marrow aspiration and biopsy were performed.
The bone marrow aspiration was performed at the posterior superior iliac spine using Klima needle. As bone marrow clots faster than peripheral blood, films are made from the aspirated material at bedside without delay. Remaining amount is transferred to an EDTA vacutainer. Usually 0.2 - 0.3 mL is sufficient for a morphological diagnosis. It has been found that more than 0.3 mL increases the peripheral blood dilution. After taking the marrow for smears, the trephine or the biopsy specimen was obtained by Jamshidi needle.
Before the biopsy specimen was transferred to 10% neutral buffered formalin, touch imprints were made by gently rolling the bony core across a clean glass slide. This along with the aspiration smears were stained with Leishmann stain. Special stains - Periodic acid Schiff stain, Myeloperoxidase, Sudan black and Perls’ stains were used wherever indicated.
Bone marrow aspirate smear
The bone marrow aspirate smear is a preparation designed to spread the cellular material of the marrow so that Leishmann stain can reveal essential cellular details.
The bone marrow aspirate is evaluated for: 1), cellularity of the fragments; 2), erythropoiesis - cellularity, maturation pattern and any cytological abnormalities; 3), myelopoiesis - cellularity, maturation pattern and any abnormalities; 4), M:E ratio; 5), megakaryopoiesis - number, morphology, presence of immature forms; 6), lymphocytes; 7), plasma cells; 8), parasites/abnormal cells/Granulomas/storage cells.
The cellularity was assessed by estimating the percentage of hematopoietic cells compared to fat spaces in the bone marrow. The categories were identified in the following way: 1), hypercellular: > 75% cells; 2), normocellular: 25-75% cells; 3), hypocellular: < 25% cells, depending upon the age of the patient.
Bone marrow biopsy
The microscopic examination of trephine biopsy is best for determining the overall cellularity and presence of infiltrates. Touch imprint preparations from the biopsy material are also useful for morphology. Trephine Biopsy Interpretation - hematoxylin and eosin sections were studied as follows: adequacy of the biopsy - the ideal specimen should be 1 - 2 cm in length, should not be distorted and should have at least 5 well preserved intertrabecular marrow spaces for interpretation.
| Results | ▴Top |
Fifty eight patients with a hematological diagnosis of pancytopenia were studied during the period October 2009 to September 2011, in the Department of Pathology, M.S Ramaiah Medical College and Hospital, Bangalore.
The following data was recorded and analyzed.
The sex distribution of pancytopenia showed a male preponderance (60%). The male to female ratio was 3:2. Most of the patients were in the age group of 21 - 30 years (25%) and least occurrence was seen in patients > 70 years (3.45%). Fever (66%) was the commonest clinical feature in pancytopenic patients. The other findings were generalized weakness (50%), pallor (46%) and easy fatigability (40%). Less common were bleeding, hepatomegaly and skin rashes (Table 1). The hemoglobin percentage varied from 3 g/dL to 10 g/dL. Majority (48%) of the patients had hemoglobin ranging from 7.1 to 10 g/dL. 47% of the patients had hemoglobin values between 4.1 and 7 g/dL. The total leucocyte count was in the range of 0.77 - 3.9 × 103/µL. Most (55%) of the patients had values in the range of 2.5 - 4.0 × 103/µL, 3% of the patients had values less than 1.0 × 103/µL. Most (78%) patients had platelet counts in the range of 50 - 100 × 103/µL.
 Click to view | Table 1. Clinical Features of Patients Presenting With Pancytopenia |
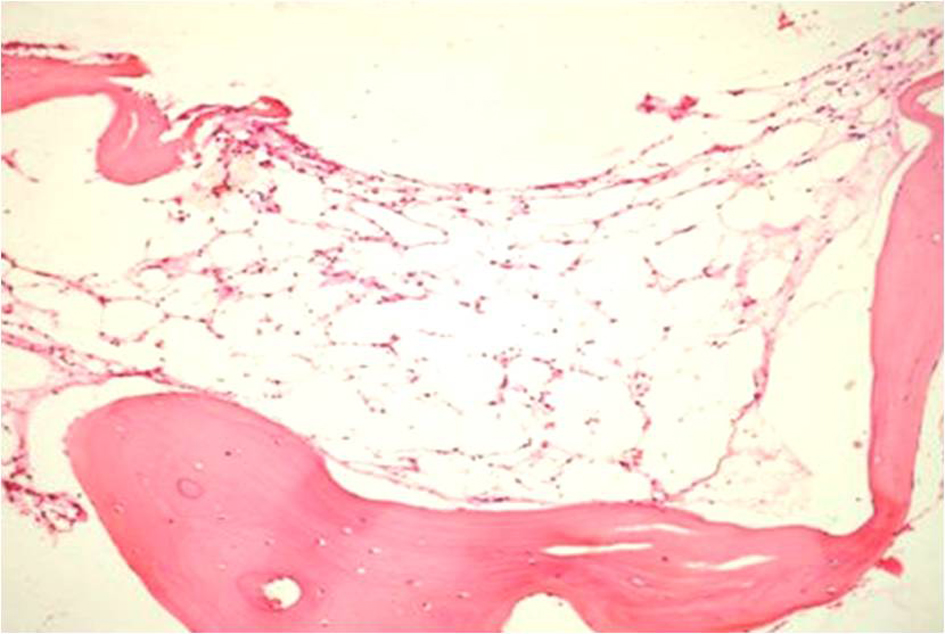
The commonest cause of pancytopenia was megaloblastic anemia (39.65%) (Fig. 1), followed by nutritional anemia (24.13%) and aplastic anemia (12.06%). The less common conditions were ALL (6.8%) and MM (5.1%). Of the 58 cases of pancytopenia, 46 (79%) were non neoplastic and 12 (21%) were neoplastic conditions. Of the 12 cases of neoplastic conditions, acute lymphoblastic (ALL) was the commonest cause (33.33%), followed by multiple myeloma (25%) (Fig. 2). The other causes were acute myeloid leukemia (AML), Waldenstrom’s Macroglobulinemia, hairy cell leukemia (HCL), Hodgkin lymphoma (HL) and metastasis (Table 2) (Fig. 3).
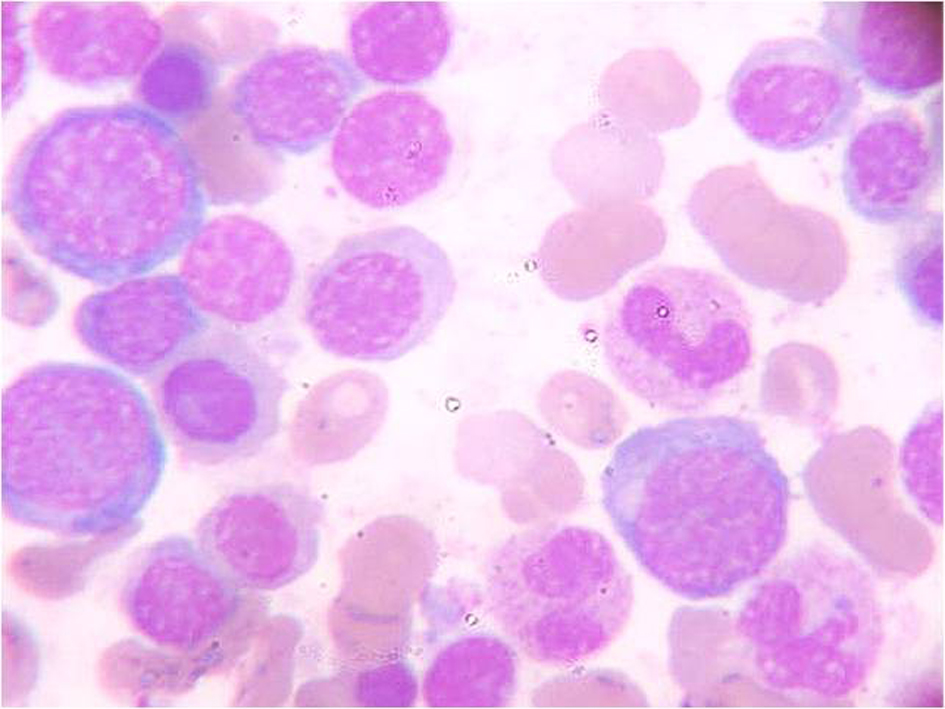 Click for large image | Figure 1. BMA showing Megaloblastic and normoblastic maturation, (Leishmann stain 100 ×). |
 Click for large image | Figure 2. BMB showing a hypocellular marrow, (Hematoxylin and eosin stain 10 ×). |
 Click to view | Table 2. Causes of Pancytopenia (n = 58) |
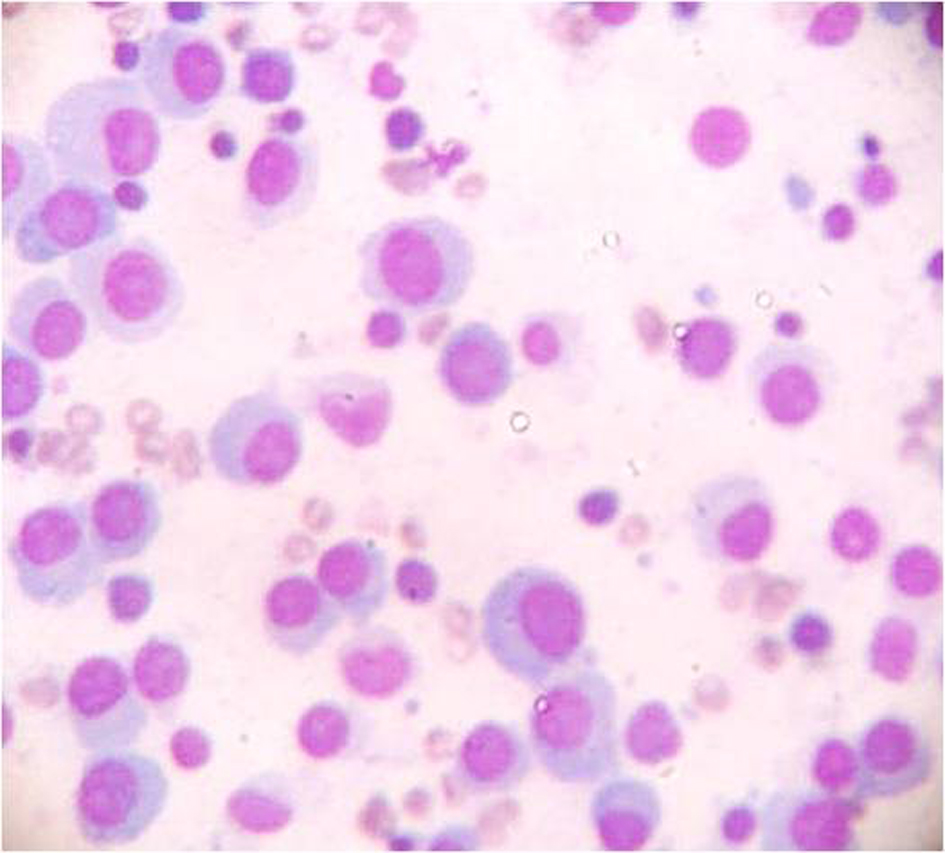 Click for large image | Figure 3. BMA showing neoplastic plasma cells, (Leishmann stain 40 ×). |
Of the 58 patients of pancytopenia, 30 (51.72%) cases had a hypercellular marrow, 21 (36.02%) a normocellular marrow. The remaining seven had hypocellular marrow (Table 3) (Fig. 4). Only one patient of hemophagocytic syndrome (HPS) was diagnosed on BMA as the biopsy was inadequate, 46 out of the total 58 cases (75.8%) showed a positive correlation (P value < 0.05). There were 2 cases (3.4%) where a definitive opinion could not be given on either BMA or BMB (Table 4).
 Click to view | Table 3. Bone Marrow Cellularity |
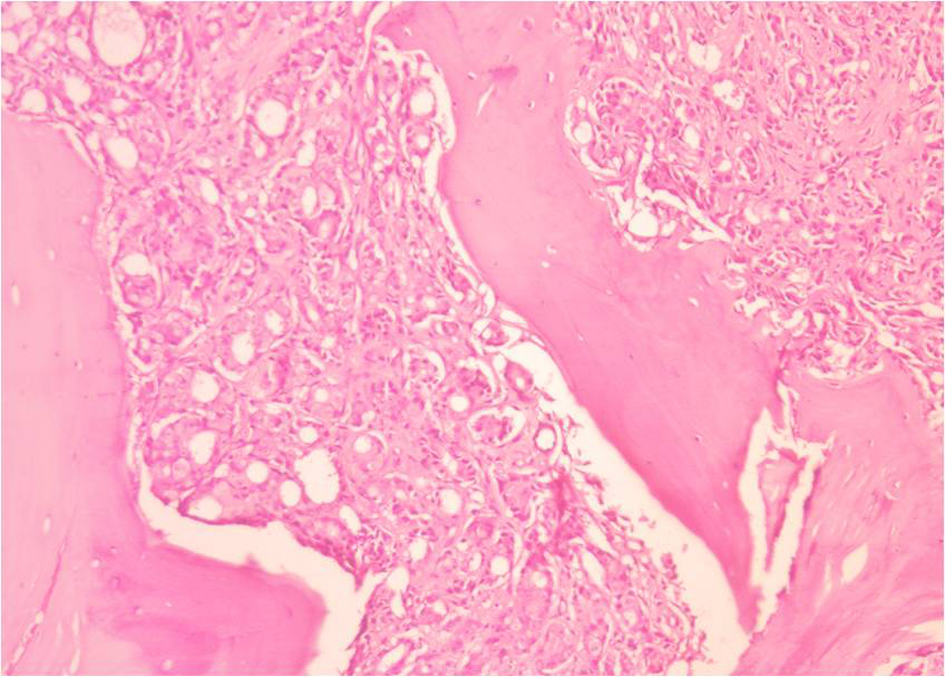 Click for large image | Figure 4. BMB showing metastatic adenocarcinoma, (Hematoxylin and eosin stain 40 ×) |
 Click to view | Table 4. Positive Correlation Between Bone Marrow Aspiration and Bone Marrow Biopsy |
| Discussion | ▴Top |
In the present study, megaloblastic anemia (39.5%) was the commonest cause of pancytopenia, followed by nutritional anemia (24.1%), aplastic anemia (12.06%), malignant diseases (18.9%), and others (5.4%). Others included uncommon causes like malaria and hemophagocytic syndrome.
Tilak V, Jain R (1998) found megaloblastic anemia (68%) to be the commonest cause of pancytopenia followed by aplastic anaemia (7.7%) [6]. Kumar et al (1999) found hypoplastic anemia (29.5%) to be the commonest cause followed by megaloblastic anemia [7].
Khodke et al (2000) observed megaloblastic anemia (44%), followed by hypoplastic anemia (14%) as the common causes of pancytopenia [3]. Mobina Ahsan Sodhy (2005) found megaloblastic anemia (35.9%) followed by hypersplenism (16.3%) as the common causes. Jha A et al [8] (2008) found hypoplastic bone marrow (29%) followed by megaloblastic anemia (23.64%) as the common cause. The commonest cause of pancytopenia, reported from various studies throughout the world has been aplastic anemia, which is in sharp contrast to results in the present study; here the commonest cause was megaloblastic anemia. This seems to reflect the higher prevalence of nutritional anemia in Indian subjects.
The commonest clinical feature was that of fever (66%), followed by generalized weakness (50%). Anemia leads to fatigue, whereas neutropenia to increased susceptibility to infections which cause fever. The findings in this study were similar to those found by Shano Naseem et al where fever (51.8%) was the commonest clinical feature. Pancytopenia is more common in males. The male: female ratio in this study was 3:2, which is similar to a study by Shano Naseem et al (2010) where also the male:female ratio was found to be 3.2:1 [9].
The non neoplastic conditions like megaloblastic anemia, nutritional anemia and aplastic anemias were more common than the neoplastic conditions like acute leukemia, which is consistent with other studies.
The hematological parameters were usually nonspecific in many cases and showed considerable overlap. In all these cases a peripheral blood film was of paramount importance in pointing towards a diagnosis of megaloblastic anemia or leukemia. Bone marrow aspiration and bone marrow biopsy are important diagnostic tools in the diagnosis of various hematological disorders, including pancytopenia. It is well known that both the procedures are complimentary to each other. Pampa Ch Toi et al (2010) found a positive correlation in 61.25% of cases when simultaneous BMA and BMB were performed. They found that the highest correlation was seen with reactive marrow and erythroid hyperplasia [10].
There was 75.8% positive correlation between BMA and BMB in the present study. The highest correlation was seen in cases of megaloblastic anemia and with erythroid hyperplasia. The erythroid series were showing either normoblastic and/or micronormoblastic maturation. On further evaluation these cases were found to be iron deficiency or megaloblastic anemia and were finally categorized as nutritional anemia.
Usually only a BMA is performed in cases of megaloblastic anemia, but as these cases presented with pancytopenia both the procedures were performed simultaneously. Many studies done previously showed that BMB was a better procedure for metastatic tumor [10]. There was single case of metastasis in the present study which was diagnosed on BMB.
Other cases which were diagnosed on BMB included acute lymphoblastic leukemia, hairy cell leukemia and Hodgkin lymphoma. In these cases there was a reactive marrow or the aspirate was diluted. These findings are consistent with those of Moid et al where they reported 95% of diagnosis of Hodgkin lymphoma by BMB alone [11]. Ramon Andrade Bezerra deMello et al reported a rare case of a patient that first presented with fever and pancytopenia due to hemophagocytosis associated with Hodgkin lymphoma (HL) [12].
In the present study seven cases had imprint smears. Rarely, the touch imprints of biopsy cores were necessary to establish a diagnosis. Touch preparations yield more certain identification of individual cells than do biopsy sections and are less likely than marrow smears to disrupt syncytial masses or compact clusters of cells [1]. It is felt that ideally an imprint smear should be obtained for the correct morphology of cells, especially if the aspirate is not good.
Conclusion
Pancytopenia is a common hematological entity that we come across in routine practice. There are numerous causes of pancytopenia which include both non neoplastic and neoplastic conditions. Clinical findings and peripheral smear findings provide valuable information in the workup of patients presenting with pancytopenia and also in planning for further investigations.
Bone marrow examination which includes BMA and BMB is an essential pre requisite for its diagnosis. Though the advantage of each procedure differs, both the procedures are complimentary to each other and should be performed simultaneously along with an imprint smear for a complete bone marrow workup and evaluation.
Megaloblastic anemia was the commonest cause of pancytopenia in the present study. Most other studies have reported aplastic anemia as the commonest cause. This seems to reflect higher prevalence of nutritional anemia in the Indian subjects. Rare causes like malaria should be kept in mind while making a diagnosis.
Source(s) of Support
Nil.
Presentation at a Meeting
None.
Conflicting Interest
None.
| References | ▴Top |
- Wintrobes. Examination of blood and bone marrow. In: Sherrie L Perkins editors. Clinical Haematology. 10th ed. Maryland: Williams and Wilkins; 1999. pp. 23- 32.
- Shirlyn B. Structure and Function of Haematopoietic System. In: Annette I Schlueter editors. McKenzie Clinical Laboratory Haematology. New Jersey: Pearson Education publishers; 2004. pp. 43- 46.
- Kishore Khodke, S Marwah, G Buxi, RB Yadav, NK Chaturvedi. Bone Marrow Examination in Cases of Pancytopenia. Journal of Indian Academy of Clinical Medicine 2001;1: 55-59.
- Gupta V, Tripathi S, Tilak V, Bhatia BD. A study of clinico-haematological profiles of pancytopenia in children. Trop Doct. 2008;38(4):241-243.
doi pubmed - Dacie and Lewis. Bone marrow biopsy. In: Imelda Bates editors. Practical Haematology. 10th ed. Philadelphia: Elsevier publication; 2006.pp.115- 118.
- Tilak V, Jain R. Pancytopenia—a clinico-hematologic analysis of 77 cases. Indian J Pathol Microbiol. 1999;42(4):399-404.
pubmed - Kumar R, Kalra SP, Kumar H, Anand AC, Madan H. Pancytopenia—a six year study. J Assoc Physicians India. 2001;49:1078-1081.
pubmed - Jha A, Sayami G, Adhikari RC, Panta AD, Jha R. Bone marrow examination in cases of pancytopenia. JNMA J Nepal Med Assoc. 2008;47(169):12-17.
pubmed - Naseem S, Varma N, Das R, Ahluwalia J, Sachdeva MU, Marwaha RK. Pediatric patients with bicytopenia/pancytopenia: review of etiologies and clinico-hematological profile at a tertiary center. Indian J Pathol Microbiol. 2011;54(1):75-80.
doi pubmed - Toi P, Varghese RG, Rai R. Comparative evaluation of simultaneous bone marrow aspiration and bone marrow biopsy: an institutional experience. Indian J Hematol Blood Transfus. 2010;26(2):41-44.
doi pubmed - Moid F, DePalma L. Comparison of relative value of bone marrow aspirates and bone marrow trephine biopsies in the diagnosis of solid tumor metastasis and Hodgkin lymphoma: institutional experience and literature review. Arch Pathol Lab Med. 2005;129(4):497-501.
pubmed - de Mello RA, Fonseca E, Brochado M, Quinaz JM. Hemophagocytic Syndrome Associated with Hodgkin's Lymphoma First Presenting as Fever and Pancytopenia. Case Rep Med. 2010;2010:759651.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.