| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Case Report
Volume 4, Number 4, December 2015, pages 242-245
Primary Bone Marrow B-Cell Lymphoma: Correlation of Results of Flow Cytometry and Morphological Findings
Monika Guptaa, b, Shalini Shaha, Nisha Marwaha, Megha Kathuriaa, Sonia Chhabraa, Rajeev Sena
aDepartment of Pathology, Pt. BDS, PGIMS, University of Health Sciences, Rohtak, India
bCorresponding Author: Monika Gupta, 17/8 FM, Medical Enclave, PGIMS, Rohtak, Haryana, India
Manuscript accepted for publication November 23, 2015
Short title: Primary Bone Marrow B-Cell Lymphoma
doi: http://dx.doi.org/10.14740/jh234w
| Abstract | ▴Top |
Primary isolated bone marrow disease as presenting feature of non-Hodgkin’s lymphoma (NHL) is very rare. We describe an elderly patient who presented with pancytopenia and was initially diagnosed as acute leukemia on the basis of morphology on peripheral blood. Flow cytometry (FCM) showed light chain restriction. Later on bone marrow biopsy along with immunohistochemistry (IHC) revealed results in concordance to FCM. Correlation of morphological findings with FCM, IHC and other ancillary techniques serves an adjunctive role in the diagnosis and classification of NHL. Immunophenotyping by flow cytometry as an auxiliary method and in correlation with morphological findings can make the diagnosis of B-cell lymphomas faster and more specific.
Keywords: Non-Hodgkin’s lymphoma; Flow cytometry; Bone marrow biopsy
| Introduction | ▴Top |
Non-Hodgkin’s lymphoma (NHL) is a biologically heterogenous disease with varied clinical presentation. B-cell NHL is the single largest category, comprising 90% of total NHL cases [1]. Secondary involvement of malignant lymphomas in bone marrow is relatively common but primary occurrence of bone marrow disease as presenting feature of NHL is quite rare [2, 3]. Primary bone marrow lymphoma (PBML) usually presents with cytopenias or fever of unknown origin raised LDH and heterogeneous histology [4].
Its early recognition is essential for establishing the accurate diagnosis and planning the treatment protocol because it is usually associated with poor prognosis [4]. Correlation of morphological findings with flow cytometry (FCM), immunohistochemistry (IHC) and other ancillary techniques serves an adjunctive role in the diagnosis and classification of NHL [5].
We describe a patient with PBML who presented with fever and pancytopenia. Due to unusual hematological manifestation in the peripheral blood, it was initially diagnosed as acute leukemia on the basis of morphology.
| Case Report | ▴Top |
A 58-year-old female presented with history of fever, generalized weakness, breathlessness and headache for 2 weeks. There was no specific past history and family history. On physical examination, she was pale and febrile. There was no lymphadenopathy and hepatosplenomegaly.
Complete blood count revealed a hemoglobin level of 6.1 g%, total leucocyte count 1.8 × 103/µL, platelet count of 2.0 × 103/µL and differential leucocyte count with neutrophils 30%, lymphocytes 26%, monocytes 4% and atypical lymphoid cells 40%. Peripheral smear revealed pancytopenia with increased rouleaux formation and presence of atypical cells. A provisional diagnosis of acute leukemia was made. Routine tests including blood coagulation profile, kidney functions, liver functions, vitamin B12 and folic acid were normal. Protein and immune electrophoresis were normal. Chest and abdominal computed tomography (CT) did not demonstrate any lymphadenopathy or hepatosplenomegaly.
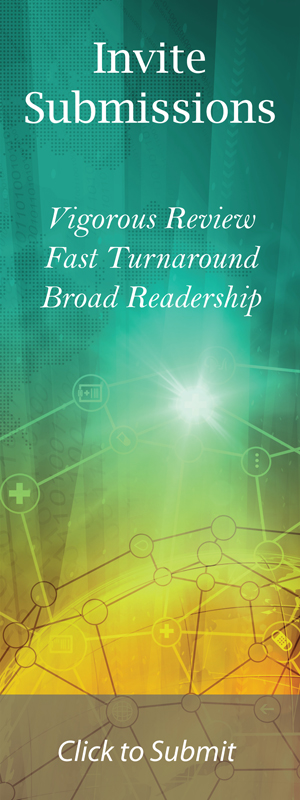
Bone marrow aspiration was done which revealed diluted marrow smears with presence of atypical cells along with plasma cells and histiocytes. Cells revealed high N/C ratio, slightly condensed nuclear chromatin with inconspicuous nucleoli and scanty amount of cytoplasm (Fig. 1).
 Click for large image | Figure 1. Peripheral blood and bone marrow aspirate revealed large sized atypical lymphoma cells with indistinct nucleoli and basophilic cytoplasm (Leishman stain, × 200). |
Immunophenotyping was performed by six-color flow cytometry using BD FACS CantoII (Becton Dickinson, San Jose, CA) on peripheral blood. CD19-gated cells showed light chain (lambda) restriction along with positivity for CD20, CD200, CD79b, and CD38. Cells showed bright CD45 while negative for CD5, CD23, CD103, CD123, FMC7, CD3, CD5, CD7, CD34 and Tdt. Although the TLC was low on peripheral blood but lambda restriction (monoclonality) on CD19 positive cells, diagnosis of B-cell NHL was made on flow (Fig. 2).
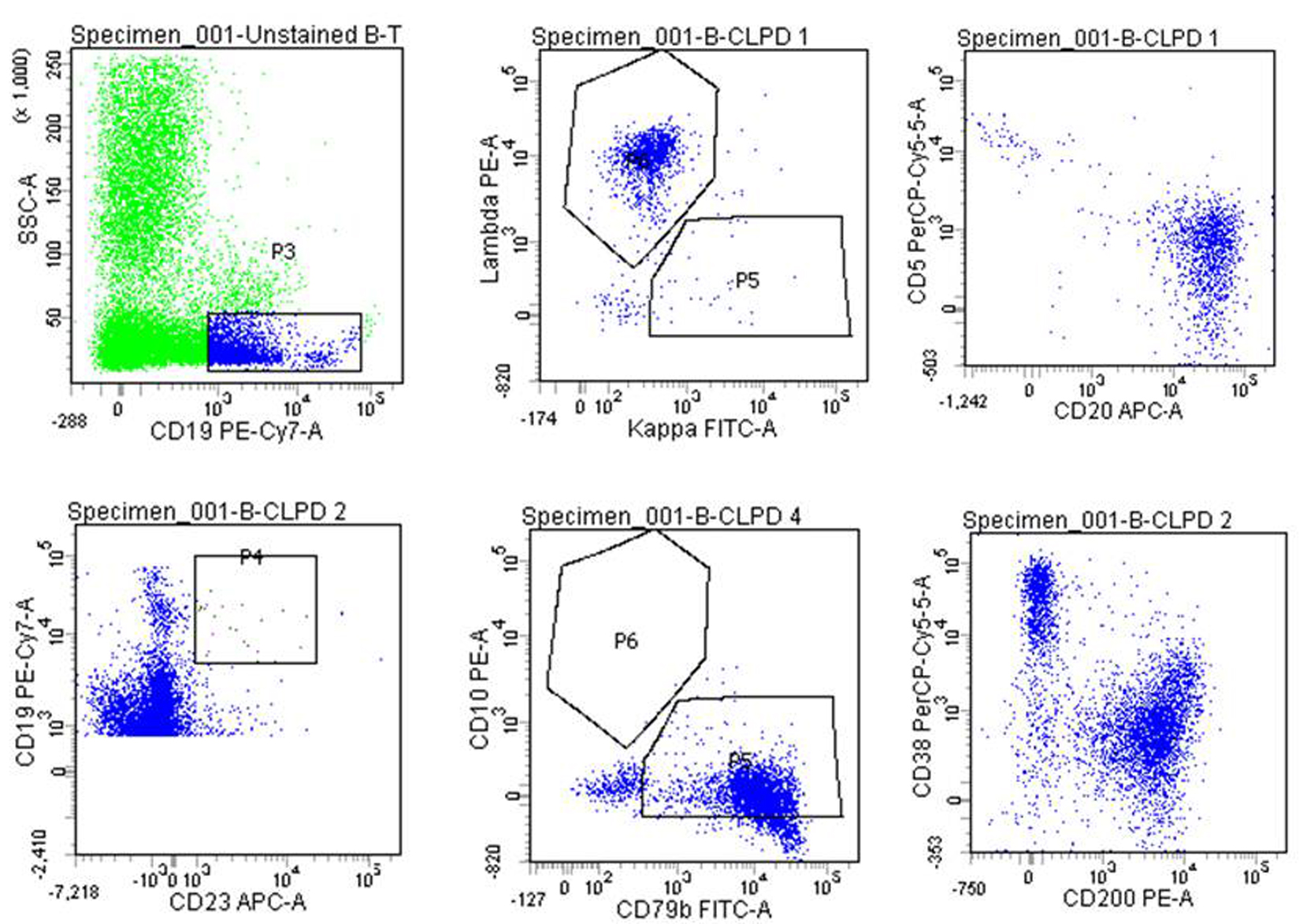 Click for large image | Figure 2. Peripheral blood immunophenotyping: (A) SSC versus CD19 gating dot plot; (B) lambda chain restriction on CD19 positive cells; (C) positive for CD20 and negative for CD5; (D) negative for CD23; (E) negative for CD10 and positive for CD79b; (F) positive for CD 200 and CD38. |
Bone marrow biopsy showed 100% cellularity and was essentially composed of atypical lymphoid cells. Normal hematopoietic elements were markedly decreased (Fig. 3). Immunohistochemistry (IHC) revealed that the cells were positive for CD 20 and CD45 while negative for CD3, CD5, CD79a, CD34 and Tdt (Fig. 4). Cytogenetic analysis revealed normal karyotype.
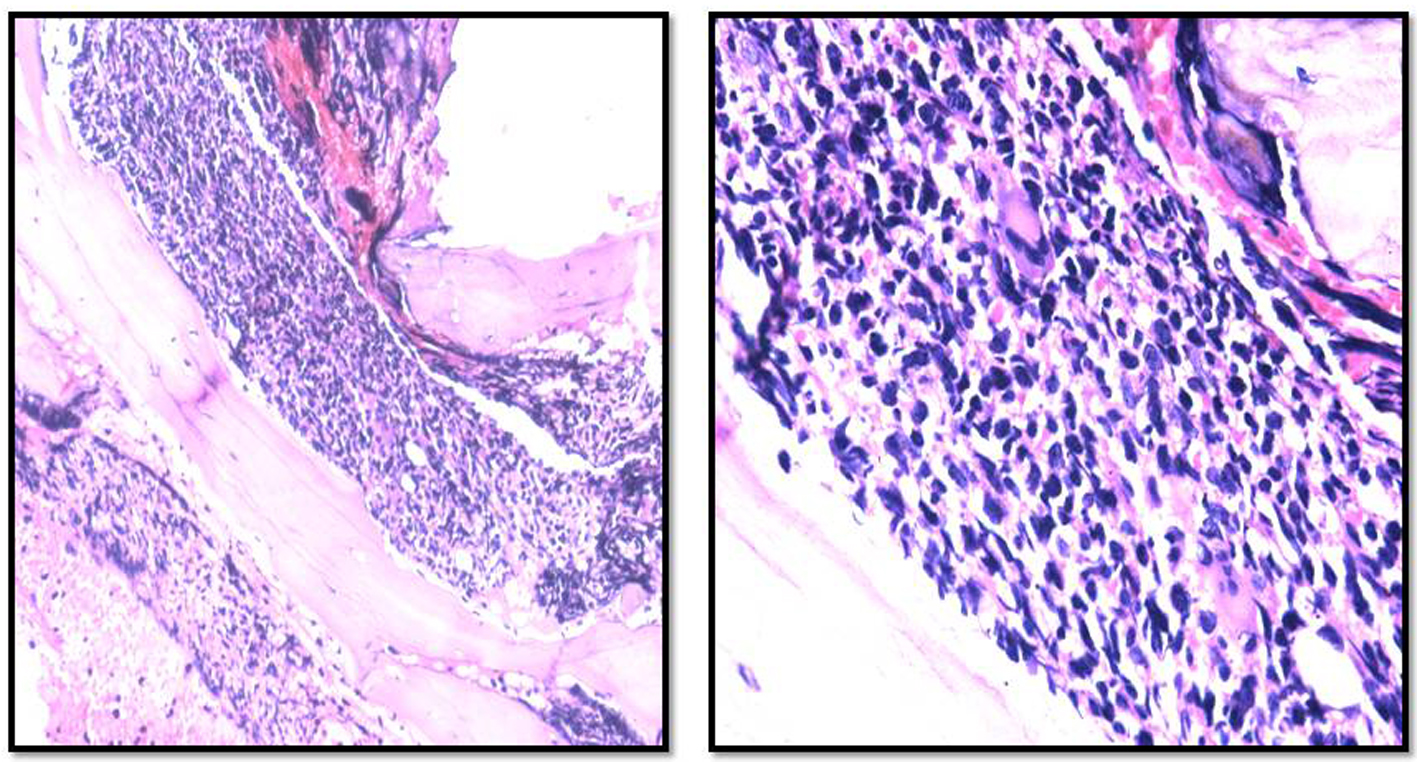 Click for large image | Figure 3. Bone marrow biopsy revealed diffuse infiltration by atypical large lymphoma cells (H&E stain, × 200, × 400). |
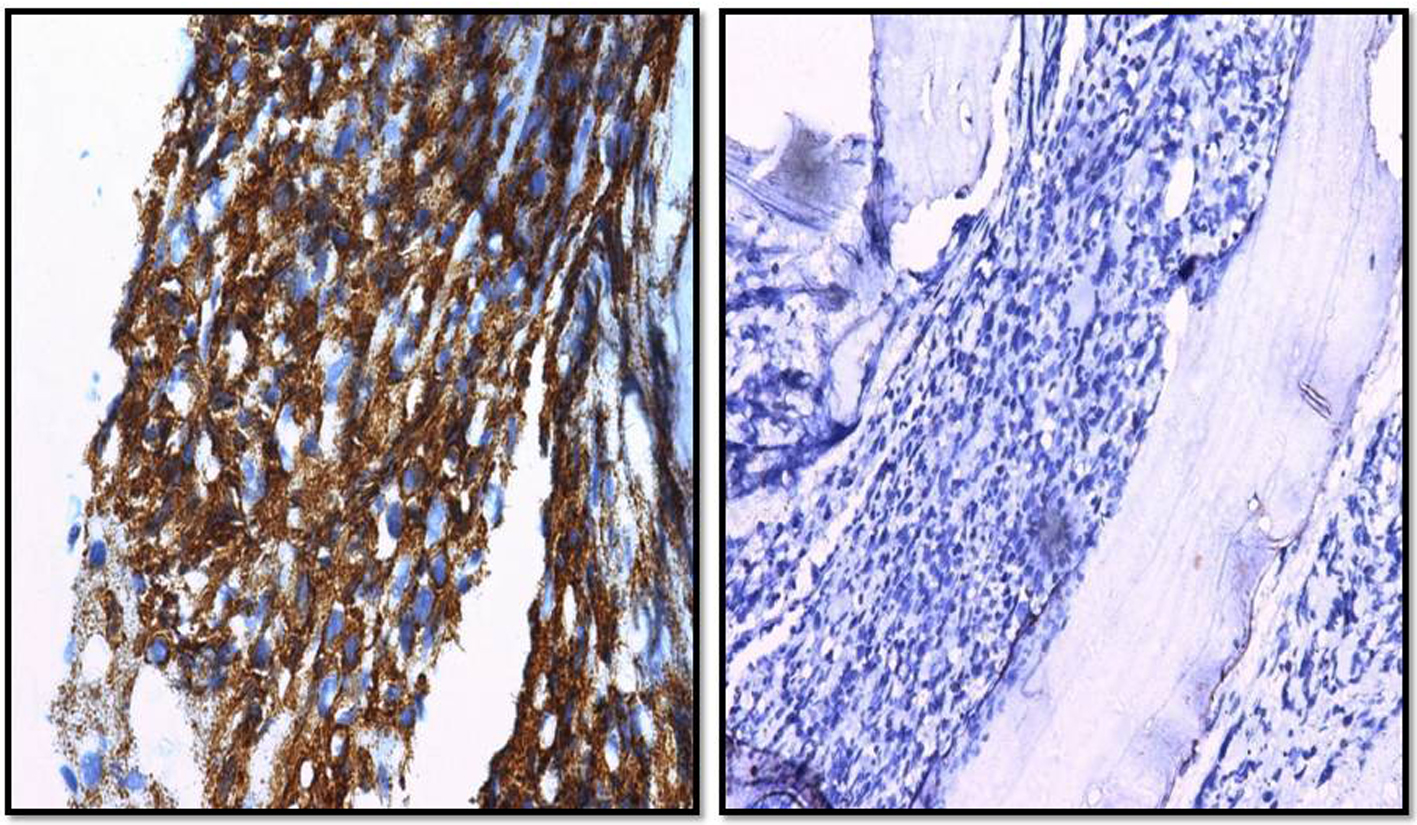 Click for large image | Figure 4. Immunohistochemical stain of bone marrow biopsy: lymphoma cells are positive for CD20 and negative for CD3 (× 400, × 200). |
Final diagnosis was achieved on the basis of combined evaluation of all modalities including the morphology, flow cytometry and IHC. The diagnosis of primary bone marrow diffuse large B-cell NHL was made. After confirmation of diagnosis, the patient was treated with R-CHOP (rituximab cyclophosphamide, doxorubicin, vincristine and prednisolone) but unfortunately patient was lost to follow-up after first cycle.
| Discussion | ▴Top |
NHL may arise at any age but are more common in the elderly. Lymphoma varies widely in its rapidity of onset and spread. Primary extranodal involvement is present in around 40% of patients at diagnosis [1]. PBML presenting with the primary bone marrow involvement is extremely rare [4]. Analysis of morphology and infiltration pattern, along with the flow cytometry and IHC investigations, is useful for narrowing down the diagnosis of PBML [6].
Recently, the diagnostic criteria of PBML have been proposed, as follows: 1) isolated bone marrow infiltration of lymphoma cells regardless of peripheral blood involvement; 2) no evidence of lymph node, spleen, liver, or other extra bone marrow involvement on physical examination or imaging studies; 3) absence of localized bone tumors; 4) no evidence of bone trabeculae destruction in the bone marrow biopsy; and 5) exclusion of leukemia/lymphoma cases [7, 8].
Review of literature revealed 53 cases of PBML. Most of the reported cases of PBML are diffuse large B-cell lymphoma. Common clinical presentation of these patients included bicytopenia or pancytopenia, fever of unknown origin, cytogenetic abnormalities, advanced lymphoma stage and raised lactate dehydrogenase levels. The cause of cytopenia was considered to be due to infiltration of marrow by lymphoma cells. Prognosis was poor in most of the reported cases [4, 6].
In our case, the patient was an elderly female who presented with fever and pancytopenia. There was no organomegaly and radiological investigations revealed normal findings. Atypical cells in the peripheral blood revealed light chain restriction on flow. Absence of lymphocytosis in the diagnostic range for chronic lymphocytic leukemia (CLL) and negative CD5, CD23 ruled out CLL while bright CD45, negative CD34 and Tdt ruled out acute leukemia in our case.
Furthermore, there was absence of localized bone tumor on CT scan and on biopsy there was no evidence of bone trabeculae destruction. Most of the marrow was replaced by these lymphoid cells which were positive for CD20 and negative for CD3 on IHC. Cause of pancytopenia in our case may be due to replacement of marrow by the lymphoid cells.
In our case, both flow cytometry and IHC were complementary to each other. The main advantage of flow cytometry is a synchronous application of two or more antibodies marked with various fluorochromes in one sample [5]. The clonality analysis provides objective and quantitative results even on very small samples or low count as in our case [9]. However, the major drawback is it requires fresh, unfixed sample and the cost especially in developing countries like us.
On the other hand, IHC works on fixed, paraffin embedded tissue and we can do morphologic analysis at the same time. But the disadvantage is evaluation of single antigens, usually one at a time, with an individual subjectivity in cases with equivocal antigen expressions.
In our opinion, both the techniques have their own advantages and disadvantages but these ancillary techniques are required for the diagnosis and classification of lymphomas along with the morphology. In atypical and unusual cases, all clinicopathologic data must be taken into consideration using a holistic approach till a satisfactory explanation of the same is found.
Conclusion
NHL should be considered in the differential diagnosis of unusual hematologic presentations as in our case, particularly in the elderly. Determination of B-cell clonality and studying co-expression profiling make the flow more sensitive and specific than IHC. Correlation of morphological findings with auxiliary method makes the diagnosis of PBML faster and more specific.
Conflict of Interests
The authors have no conflicts of interest.
| References | ▴Top |
- De Gruchy GC. Tumours of lymphoid tissues. In Firkin F, Chestermann C, Penington D (eds). De Gruchy's Clinical Haematology in Medical Practice.5th edition. Oxford University Press. 1989;257-278.
- Kajiura D, Yamashita Y, Mori N. Diffuse large B-cell lymphoma initially manifesting in the bone marrow. Am J Clin Pathol. 2007;127(5):762-769.
doi pubmed - Lee Y Ja, Kim H Jae, Shin H Jeong, Kim R Hye, Lee N Jeong, Kim H Ki, Lee S Won, Joo D Young, Sohn H Chang, Kim CH. Primary isolated bone marrow diffuse large B-cell lymphoma with hemolytic anemia as the first manifestation. Korean J Hematol. 2008;43(1):48-52.
doi - Nishida H, Hori M, Obara K. Primary isolated bone marrow diffuse large B-cell lymphoma with the initial presentation as severe thrombocytopenia, successfully treated with chemotherapy: a case report and review of the literature. Journal of Cancer Therapeutics and Research. 2012;1:28.
doi - Mand'akova P, Campr V, Kodet R. [Correlation of results of flow cytometry and morphologic findings in the diagnosis of malignant B-cell lymphoma]. Cas Lek Cesk. 2003;142(11):651-655.
pubmed - Kagoya Y, Sahara N, Matsunaga T, Uekusa T, Irie S, Hatanaka K. A Case of Primary Bone Marrow B-Cell Non Hodgkin's Lymphoma with Severe Thrombocytopenia: Case Report and A Review of the Literature. Indian J Hematol Blood Transfus. 2010;26(3):106-108.
doi pubmed - Yamashita T, Ishida M, Moro H, Yumoto H, Uchibayashi S, Yoshii M, Nakanishi R, et al. Primary bone marrow diffuse large B-cell lymphoma accompanying cold agglutinin disease: A case report with review of the literature. Oncol Lett. 2014;7(1):79-81.
pubmed - Martinez A, Ponzoni M, Agostinelli C, Hebeda KM, Matutes E, Peccatori J, Campidelli C, et al. Primary bone marrow lymphoma: an uncommon extranodal presentation of aggressive non-hodgkin lymphomas. Am J Surg Pathol. 2012;36(2):296-304.
doi pubmed - Kaleem Z. Flow cytometric analysis of lymphomas: current status and usefulness. Arch Pathol Lab Med. 2006;130(12):1850-1858.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.