| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Case Report
Volume 4, Number 4, December 2015, pages 235-237
Pseudo-Hyperkalemia and Thrombocytosis: Case Report
Monica Irani Gouveiaa, c, Luis Carlos Reis Capobiangob
aMedical School, Centro Universitario de Caratinga, UNEC, Brazil
bCentro Universitario de Caratinga, UNEC, Brazil
cCorresponding Author: Monica Irani de Gouveia, Rua Moacir de Matos, 49 Centro Caratinga, MG, CEP 35 300-000, Brazil
Manuscript accepted for publication October 13, 2015
Short title: Pseudo-Hyperkalemia and Thrombocytosis
doi: http://dx.doi.org/10.14740/jh228w
| Abstract | ▴Top |
Our case is to describe clinical and laboratory diagnosis of pseudo-hyperkalemia associated with thrombocytosis. A 78-year-old male, with prior hypertension, who previously suffered a femoral neck fracture, was presented to the orthopedic service to perform hip arthroplasty. In further evaluation, we found one hyperkalemia and serum thrombocytosis without clinical worsening and without correlated changes in the electrocardiogram (ECG). The possibility of pseudo-hyperkalemia was considered, and technical mechanical failures or problems in transportation were investigated, because it is a condition induced by hemolysis and excessive potassium leakage from the cells during or after blood collection. Using heparinized test tubes, two blood samples were collected within a 6-hour period, to which K+ levels were obtained in the normal range. In conclusion, a high number of platelets in the blood can release potassium ions to the plasma environment, causing pseudo-hyperkalemia, leading to the decision for hospitalization and inappropriate treatments.
Keywords: Anticoagulants; Thrombocytosis; Electrocardiogram
| Introduction | ▴Top |
First of all, differentiating pseudo-hyperkalemia from hyperkalemia may present a challenge for many professionals and lead to the incorrect treatment, since hyperkalemia is life-threatening to the patient and requires immediate action. Here we present a case of pseudo-hyperkalemia in an elderly patient without the typical symptoms of it, including an electrocardiogram (ECG) without amendments relating to this condition. There are several ways to promote the output of the cation K+ intracellular and its appearance in plasma or serum, without being a pathology, featuring a pseudo-hyperkalemia. In common situations such as mechanical trauma and refrigerating the material to be analyzed, the transport of test tubes to the laboratory can cause shocks on the walls and release of the intracellular cation, in blood with thrombocytosis or leukocytosis. Yet trauma could be reported to increase venous pressure at the time of blood collection. The cooling at a temperature lower than 37 °C such as releasing factor of K+ cations has also been reported in a condition called familial pseudo-hyperkalemia. Until its confirmation, the pseudo-hyperkalemia can trigger inappropriate hospitalizations and unnecessary investigations such as repetitions of laboratory tests, ECGs and inappropriate treatments, in addition to diet modifications. The aim of this study is to report a case of pseudo-hyperkalemia in an elderly patient with a hip fracture, associated with thrombocytosis, which generated treatment for hyperkalemia at first, until the team suspected pseudo-hyperkalemia and took steps to manage it.
| Case Report | ▴Top |
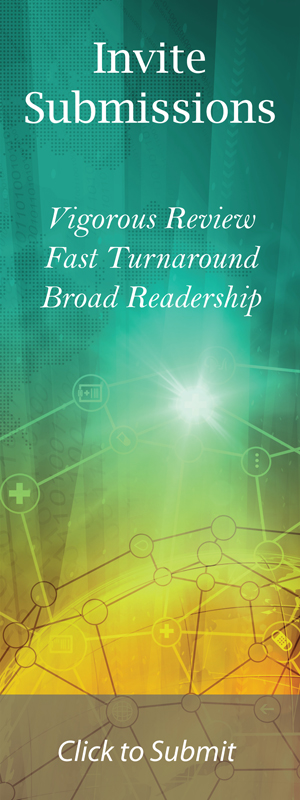
A man aged 78, with prior hypertension, who previously suffered a left femoral neck fracture, was admitted to the hospital unit, on May 13, 2015, for orthopedics services when the need to perform hip arthroplasty was discovered. He is a drinker and smoker. There were no recent changes to the drugs used at home. He was found lucid, verbalizing and with fecal and urine matter present. On admission assessment, he showed an increase of nitrogenous waste (urea and creatinine) and blood potassium levels within the normal range. He drew attention to one polyglobulia blood count with hematocrit of 54% and platelet 1.2 × 106 cells/mm3. On the 20th of this month, the opinion of a nephrologist was requested. Vital signs were within normal limits, and the physical examination was normal. The repetition of the laboratory tests confirmed the elevated serum urea and creatinine, as well as value of K+ equal to 7.6 mEq/L. The nephrologist referred the patient to the intensive care unit (ICU), and initiated management to hyperkalemia and requested an ECG. To treat the hyperkalemia, the following was used: 10% calcium gluconate, intravenous (IV), for 30 min q8h; ion exchange resin, 30 g q6h; nebulized β2 agonist (fenoterol hydrobromide), eight drops q4h; 50% glucose solution associated with regular insulin, 10 IU, IV, continuous infusion pump to run at 2 h and again after 4 h. New laboratory tests were performed, in which potassium serum dosage was 8.6 mg/dL. The patient remained clinically stable, without the classic symptoms of hyperkalemia, and ECG showed no T waves and symmetrical or absence or reduction of P waves nor increased PR interval or evidence of high-grade blockade (Fig. 1).
 Click for large image | Figure 1. ECG without evidence of changes for hyperkalemia. |
Given this situation, a pseudo-hyperkalemia was considered. To confirm this, new dosages of K+ were performed in heparinized test tube, after re-calibration of the injector device and with considerable care to minimize cell lysis, and the results were 2.6 and 5.4 mg/dL, respectively. The data are presented in Table 1.
 Click to view | Table 1. Analytical Patient’s Evolution |
During his period of hospitalization, blood pressure (BP) remained an average of 150 × 90 mm Hg; axillary temperature was around 36.0 °C; Na+ dose remained in medium 136 mEq/L. Following the care of the patient, we started to investigate the thrombocytosis and leukocytosis, whilst taking preventative action to manage kidney function.
| Discussion | ▴Top |
Hyperkalemia is an electrolyte disorder that is life-threatening, requiring immediate diagnosis and treatment. It should be differentiated from pseudo-hyperkalemia. The latter is defined as an elevation of potassium levels usually due to mechanical trauma during venipuncture, resulting in hemolysis and potassium releasing from the cellular elements of blood [1]. This is a subject not well known among scholars, with a search of the Virtual Health Library, using the keywords “pseudo-hyperkalemia”, Medline (International Literature on Health Sciences) delivers only 93 scientific articles; in IBECS (Spanish Bibliographic Index of Health Sciences), there were no publications and Scielo (Scientific Electronic Library Online) met two publications in July this year.
In the same way, Ong et al cite in their research an inadequate management of patients with myeloproliferative disorders and pseudo-hyperkalemia, finding only seven systematic studies and case reports in the literature [2]. The pseudo-hyperkalemia is a major disorder in vivo and in vitro. An interesting place is made by Bawazir et al, analyzing blood bags that remained in cooling (< 37 °C) and then were transfused in infants, obtaining potassium dosage of 33.9 and 13.76 mmol respectively, and were transfused in a newborn, as well as a 4-month-old baby. Referred to as the FP, an inherited condition in which red blood cells have increased permeability K+ ions is induced by cold [3]. In vitro example is more common: Klota et al reported their experience with a patient in a well general condition presenting hyperkalemia (K+: 9.6 mEq/L). After proper treatment, their patient has showed 5.6 and 7.6 mEq/L and no compatible ECG changes. The clinical team suspected then pseudo-hyperkalemia, and to confirm, two blood samples were sent for analysis using different types of transport, one by hand and other through routine pneumatic transport system of the hospital, revealed potassium values 3.4 and 7.8 mEq/L, respectively [1]. It is important to distinguish true hyperkalemia from pseudo-hyperkalemia, which is not well known among medical professionals and, as a result, may lead to treatment for hyperkalemia, with serious consequences for patients who do not have the condition.
Conclusion
Because of its cardio-toxic potential, real hyperkalemia is a potentially fatal abnormality, highlighting the importance of being able to differentiate it from pseudo-hyperkalemia, to determine appropriate interventions. The necessary treatment can only be determined by taking into account the clinical history, hemodynamic, appropriate clinical laboratory research and the echocardiographic findings. It is possible for release of K+ cations from the platelets to blood plasma environment, and pseudo-hyperkalemia should be investigated in patients with thrombocytosis with no clinical deterioration and/or no ECG evidence of hyperkalemia. In this situation, it is recommended to investigate technical or mechanical causes such as collection with high pressure on the vein or pneumatic conveying test tubes. To conclude, these problems has fast and affordable solutions such as proper calibration of the dispensing devices, the collection with proper tourniquet, the use of anticoagulants and transport without shaking or vibration, among others. These measures also represent gains for the patient and medical staff, as bordering eventual failure and preventing inappropriate treatment.
| References | ▴Top |
- Kotla S, Makhoul S, Gonzalez III L. Pseudohyperkalemia from a pneumatic tube transport system: case report and literature review. Hospital Pharmacy. 2012;47(5):371-374. doi: 10.1310/hpj4705-37. www.thomasland.com.
- Ong YL, Deodore R, El-Agnaf M. Pseudohyperkalaemia is a common finding in myeloproliferative disorders that may lead to inappropriate management of patients. International Journal of Laboratory Hematology. 2010;2:151-157.
doi - Bawazir WM, Flatt JF, Wallis JP, Rendon A, Cardigan RA, New HV, Wiltshire M, et al. Familial pseudohyperkalemia in blood donors: a novel mutation with implications for transfusion practice. Transfusion. 2014;54(12):3043-3050.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.