| Journal of Hematology, ISSN 1927-1212 print, 1927-1220 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Hematol and Elmer Press Inc |
| Journal website http://www.thejh.org |
Original Article
Volume 3, Number 1, March 2014, pages 1-9
Tissue Doppler Echocardiography in Detection of Myocardial Iron Overload Confirmed by Cardiac MRI in Patients With Beta Thalassemia Major: A Meta-Analysis
Rozelle Jade Javiera, Flordeluna Zapata-Mesinab, c, Ma Rosario Irene D. Castillob
aDepartment of Medicine, University of Santo Tomas Hospital, Manila, Philippines
bDepartment of Medicine, Section of Hematology, University of Santo Tomas Hospital, Manila, Philippines
cCorresponding author: Flordeluna Zapata-Mesina, Department of Medicine, Section of Hematology, University of Santo Tomas Hospital, Manila, Philippines
Manuscript accepted for publication December 14, 2013
Short title: Tissue Doppler Echocardiography
doi: https://doi.org/10.14740/jh107w
| Abstract | ▴Top |
Background: Myocardial iron overload is the most serious complication seen in transfusion-dependent beta thalassemia. Congestive heart failure remains to be the leading cause of death in thalassemia major patients. It is therefore important to facilitate early detection of myocardial iron overload in affected patients to avoid inevitable complications of treatment. Cardiac magnetic resonance imaging (MRI) continues to be the gold standard in detecting myocardial iron overload as it is the most sensitive and most precise imaging procedure available. It is however expensive, time-consuming and not universally available in all institutions. These reasons preclude it from being widely utilized in our practice. Tissue Doppler echocardiography on the other hand is widely available, faster and has significantly lower costs than the latter. These characteristics make it a promising alternative diagnostic tool for detection of and screening for cardiac iron overload. This study aims to determine the correlation of tissue Doppler echo parameters compared to the current gold standard, cardiac MRI T2 star.
Methods: A literature search of published English language studies was performed using PubMed, MEDLINE and the Cochrane Collaboration from 1990 to 2013. Articles included were prospective cross-sectional and case-control trials. The risk of bias assessment (PRISMA) feature of Revman 5.0 and the QUADAS criteria were used to qualify for validity of the said qualified studies.
Results: Five prospective observational studies were included with a total of 276 subjects. Four tissue Doppler parameters were analyzed and compared to cardiac MRI T2* findings. Results showed that patients with some degree of iron overload, evident in CMR T2* < 20 ms, had a statistically significant decrease in left ventricular ejection fraction (LVEF) with an overall mean difference (MD) of -3.84 (-5.85, -1.83) (Z = 3.75, P = 0.0002); increased Tei index (MD 13.03 (9.77, 16.99), Z = 7.83, P < 0.00001); and shorter deceleration times (MD -27.10 (-33.50, -20.71), Z = 8.31, P < 0.00001). There was no difference in E/A ratio of normal subjects versus iron overloaded patients (MD 0.18 (0.09, 0.27)) and therefore is not a reliable parameter to gauge myocardial iron overload (Z = 3.88, P = 0.0001).
Conclusion: Tissue Doppler parameters that were seen to have good correlation with cardiac MRI T2*, the current gold standard, are Tei index, deceleration time and LVEF.
Keywords: Tissue Doppler echocardiography; Myocardial iron; Overload; Cardiac MRI; Beta thalassemia; Meta-Analysis
| Introduction | ▴Top |
Beta thalassemia is a group of autosomal recessive hematologic disorders that results from the defective production of beta-globin chains of hemoglobin. The homologous state of this genetic defect, thalassemia major (TM), causes transfusion-dependent anemia in affected patients. In otherwise heterozygous states, it usually causes mild to moderate microcytic anemia. This condition is most commonly found in the Mediterranean region, Africa and Southeast Asia, presumably in association with the incidence of endemic malaria [1]. From data in 2011 by the Thalassemia Center of the Philippines and Balikatang Thalassemia, the incidence of beta thalassemia is relatively low (< 1%) compared to other hemoglobinopathies, this may however be underestimated [2]. There is nevertheless a growing number due to increasing awareness and improvement in diagnostic capabilities of the different medical centers. The most common gene mutation is the “Filipino” deletion accounting for 45.8% (27/59) of the studied alleles, in a study conducted by Ko et al [3]. Although the burden of beta thalassemia arises mainly from the hematologic pathology itself such as hemolytic anemia, skeletal abnormalities even during early infancy and poor growth, a significant number of complications arise from its treatment especially in transfusion-dependent beta thalassemia.
In TM patients, blood transfusion requirement can start as early as the first few months of life. It is lifesaving in majority of patients; however, it also comes with risks of infections and iron overload. Iron overload is the most dreaded complication of chronic blood transfusions and most commonly affects the heart and the liver. Myocardial iron overload eventually leads to congestive heart failure in affected patients and results to be the most common cause of mortality in this population. The incidence of iron overload cardiomyopathy ranges from 11.4% to 15.1% in TM patients [4, 5]. Restrictive cardiomyopathy usually occurs before dilated cardiomyopathy, in accordance with diastolic dysfunction, which normally happens before systolic dysfunction and overt heart failure. Left-sided heart failure is clinically more common than right-sided heart failure. However, it has been shown that right ventricular dysfunction develops earlier in asymptomatic TM patients [6-8]. Early recognition of patients at risk for heart failure is vital since early initiation of iron chelation therapy has been shown to prevent progression or even reverse the adverse of iron-induced cardiomyopathy. Once heart failure has been clinically evident, it is already difficult to reverse this complication despite aggressive iron chelation [9].
Cardiac magnetic resonance imaging (MRI)
Iron-induced cardiomyopathy is reversible if timely diagnosed and chelation therapy is instituted. Unfortunately, myocardial iron overload cannot be predicted by conventional tests like serial determinations of serum ferritin or even with correlation of liver iron content. The option of cardiac biopsy for iron quantification is likewise not recommended because of safety considerations, sampling error and patchy nature of iron deposition in the myocardium [10]. Magnetic resonance represents the imaging method of choice for monitoring iron overload in the heart. It can indirectly quantify myocardial iron content by the paramagnetic effects of stored iron in the form of ferritin and hemosiderin. Interaction with nearby hydrogen nuclei in tissue water produces changes in the MR signal intensity, susceptibility variability and shortens relaxation times T1, T2 and T2* [10]. Over the last few years, cardiac MRI has become the gold standard for making the diagnosis of myocardial iron overload, by the specific index of myocardial relaxation time, T2*. According to a review by Kondur et al, CMRI T2* can be used for the preclinical detection of myocardial iron overload and likewise monitoring of myocardial iron content during chelation therapy [10].
MRI changes consistent with the reduction of cardiac iron that are paralleled by improvement in cardiac function have been reported in a number of studies [11]. Although the current gold standard for quantification of myocardial iron, cardiac MRI is still not widely available in most institutions. Along with its relatively high cost, this limits its use in developing countries, such as the Philippines. This led to the investigation for other imaging modalities that may detect early signs of cardiac iron overload before the development of overt cardiomyopathy.
Tissue Doppler echocardiography (TDE)
TDE has become an established arm of diagnostic ultrasound examination. It allows demonstration and assessment of myocardial contraction using Doppler technology, often with color coding. It uses frequency shift of ultrasound waves to calculate myocardial velocity. Two techniques are used to assess myocardial function: pulsed TDE and color-coded TDE, which is an extension of the former. Pulsed-wave TDE is used to measure peak myocardial velocities and is used to measure long-axis ventricular motion. With color-coded TDE, a color-coded representation of myocardial velocities is superimposed on gray-scale two-dimensional or M-mode images to indicate the direction and velocity of myocardial motion. It has the advantage of increased spatial resolution and ability to evaluate multiple structures in a single view.
Several studies have been conducted to assess the usefulness of TDE in detection of myocardial iron overload. Results of individual studies have given contradicting results in comparison to cardiac MRI. Majority of the studies have regarded parameters of diastolic function as more sensitive indices of myocardial iron loading, however are yet overall inconclusive. In a study by Olivier et al, it was found that diastolic dysfunction in asymptomatic individuals has been shown to have prognostic significance for the development of symptomatic iron-induced cardiac disease in some studies [11].
| Materials and Methods | ▴Top |
Literature search strategy
An extensive literature search of published studies from 1990 to 2013 was reviewed from PubMed and MEDLINE online databases as well as from the Cochrane Collaboration Library on the use of tissue Doppler in screening beta thalassemia patients with probable myocardial iron overload. The following keywords were used: “tissue Doppler”, “cardiac mri”, “iron overload”, “beta-thalassemia” and “transfusion”. All matches from the search were appraised by titles and those relevant to the study were included initially in the appraisal.
Retrieved articles including full articles and abstracts were reviewed and those with missing or unpublished data were excluded. A total of 35 studies were retrieved and appraised in accordance with the above inclusion and exclusion criteria. Out of the 35 studies, 21 were further excluded based on screening the titles and abstracts. Two citations did not have abstract. Upon trying to make a correspondence with the author, the researchers have yielded no reply. Three citations were not published in English and cannot be retrieved. The remaining nine articles were then assessed for eligibility using the PRISMA statement. Since the studies included were not randomized controlled trials, the Jadad scoring system was not used, instead, the risk of bias assessment (PRISMA) feature of Revman 5.0 and the quality assessment of studies of diagnostic accuracy (QUADAS) criteria were used to qualify for validity (Fig. 1).
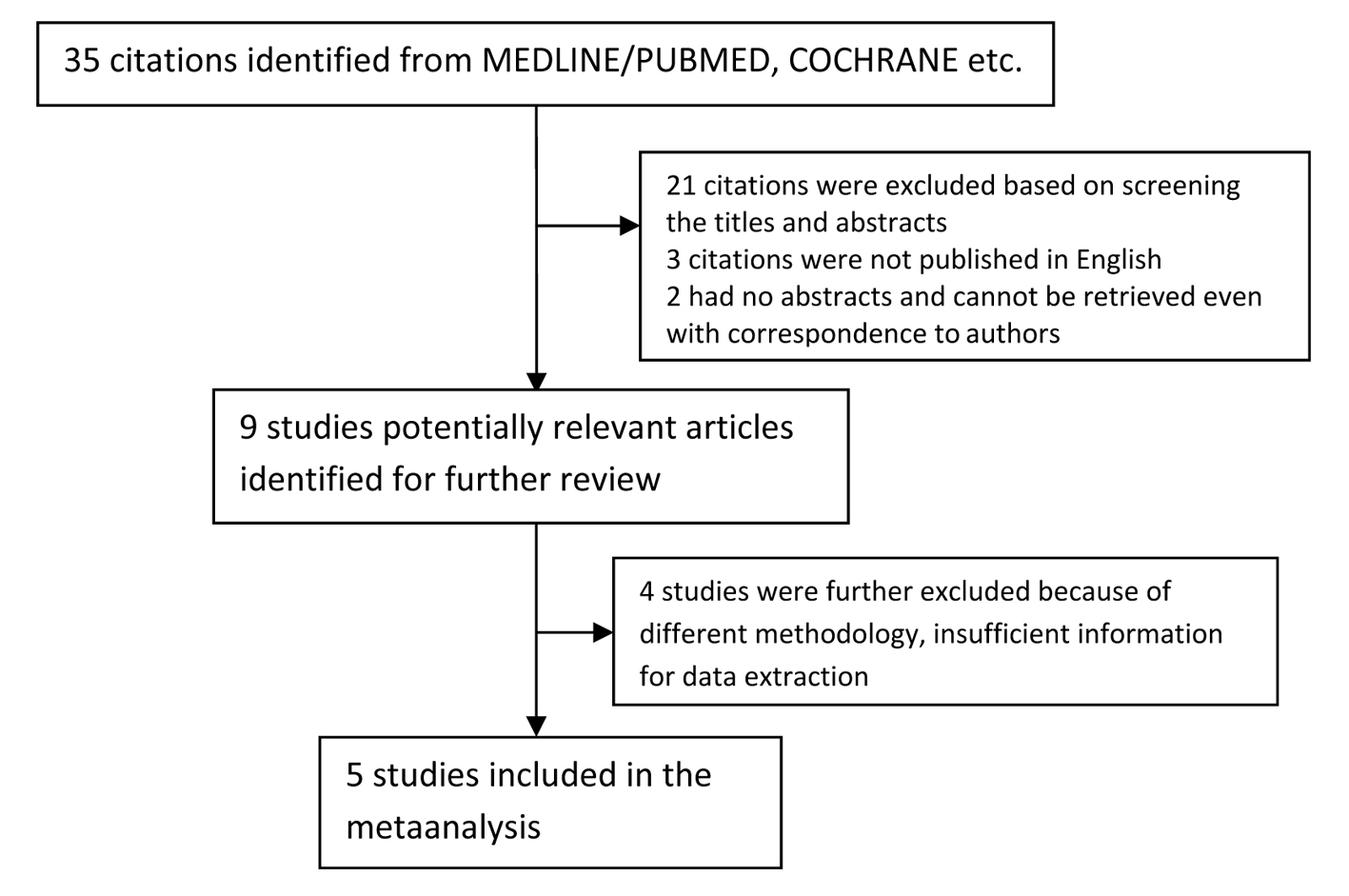 Click for large image | Figure 1. Flowchart of study selection. |
Inclusion and exclusion criteria
We reviewed abstracts of all citations and retrieved studies. The following criteria were used to include published studies: 1) studies evaluating the usefulness and reliability of tissue Doppler in screening for myocardial iron overload in beta thalassemia major patients on transfusion therapy; 2) studies used cardiac MRI to confirm iron overload in the subjects being studied; 3) parameters measured include left ventricular ejection fraction (LVEF), Tei index, E/A ratio and deceleration time (DT); 4) prospective trials. Studies were excluded if one of the following existed: 1) insufficient information for extraction of data; 2) unpublished results.
Analyzed studies
We reviewed results of trials evaluating tissue Doppler imaging (TDI) compared to cardiac MRI (CMRI) T2* in screening for myocardial iron overload in transfusion-dependent TM patients. Data sources included prospective cross-sectional and case-control trials published between January 1990 and January 2010, as described previously (keywords: tissue Doppler index, Cardiac Magnetic Resonance Imaging, Beta-Thalassemia Major, Iron overload).
Data extraction
All data were extracted independently by 2 reviewers according to the inclusion criteria listed above. Disagreements were resolved by discussion between the reviewers. Subject demographics were compared and checked for homogeneity (Table 1). The following characteristics were also collected from each study: first author, year of publication, country of the first or corresponding author, number of cases and controls and diagnostic methods (Table 2).
 Click to view | Table 1. Demographics |
 Click to view | Table 2. Characteristics of Included Studies |
Statistical analysis
The meta-analyses evaluated the application of tissue Doppler as a screening tool in detecting myocardial iron overload among TM patients on regular transfusion as confirmed by cardiac MRI. Effect estimates for mean difference (MD) in LVEF, Tei index, E/A ratio and DT along with their corresponding confidence intervals were derived from RevMan 5.0 and calculated with fixed-effects models. Forrest plots were generated using the same platform. All statistical tests were two-sided and effect estimates were deemed statistically significant when P ≤ 0.05.
Studies included in the meta-analysis
The efficacy of tissue Doppler imaging in predicting myocardial iron load in patients with beta-thalassemia major: correlation with T2* cardiovascular magnetic resonance. Aypar E, Alehan D, Hazirolan T, Gumruk F
In this study by Aypar et al, they investigated on the value of TDI in detection of iron-induced myocardial dysfunction, as compared to T2* cardiac MRI. In this case-control study, 33 asymptomatic TM patients with normal left ventricular global systolic function (ejection fraction > 55% and fractional shortening > 30%) were included and compared them to 20 healthy age- and sex-matched controls. The two groups were evaluated using conventional echocardiography and pulsed-wave TDI. Any complaints that may be attributed to a cardiovascular disease or any risk of developing such (evidence of arrhythmia, history of smoking, diabetes, hypertension or renal disease, and so on) were grounds for exclusion from the study. It was concluded that TDI can detect regional systolic and diastolic myocardial dysfunction earlier than global dysfunction in thalassemia patients. Although CMRI T2* is still the most sensitive test, TDI can be used for screening of patients in identifying myocardial iron load. This study was also able to identify cut-off values in predicting presence of myocardial iron load and cut-off values for determining the presence of severe myocardial iron load [12].
Correlation of cardiac MRI T2* with echocardiography in thalassemia major. Barzin M, Kowsarian M, Akhlaghpoor S, Jalalian R, Taremi M
This cross-sectional study included 33 TM patients with at least a 15-year history of blood transfusion. All patients were negative for heart failure symptoms. All cases underwent CMRI T2* followed by echocardiography with systolic and diastolic evaluation and TDI. Through good correlation between MRI and echocardiographic parameters (DT, E/Em and Tei index), this analysis was able to conclude that TDI may be an option for evaluation of myocardial iron overload, especially in developing countries. Although not fully replacing CMRI for diagnosis of myocardial siderosis, it offers TDI as an adequate means of monitoring for disease progression and response to iron chelation therapy with a baseline study along with initial T2* evaluation [9].
Evaluation of diagnostic power of tissue Doppler echocardiography for assessment of cardiac iron overload in patients with thalassemia major. Dabirian M, Jalalian R, Karami H, Kowsarian M, Ahmadi A, Shokohi L, Alizadeh R
This study aims to determine the efficacy, specificity and thus diagnostic value of TDE in assessing myocardial iron load as compared to the current gold standard cardiac MRI T2*. In this cross-sectional study, a total of 50 TM patients aged 15 years old and above were asked to undergo cardiac MRI followed by TDE. Several echocardiographic parameters of diastolic and systolic dysfunction were measured and correlated with cardiac MRI findings. This study was able to conclude that diastolic cardiac dysfunction demonstrated by TDE has a significant association with MRI results. On the other hand, systolic dysfunction was shown to have poor correlation with myocardial iron deposition. Through data presented in this study, it was recommended to use evaluation of diastolic cardiac function via TDE as an early and more sensitive index to predict iron deposition [13].
Correlation of echocardiography parameters with cardiac magnetic resonance imaging in transfusion-dependent thalassaemia major. Aessopos A, Giakoumis A, Fragodimitri C, Karabatsos F, Hatziliami A, Yousef J, Gotsis E, Berdoukas V, Karagiorga M
In this analysis, Aessopos et al assessed 142 thalassemia patients for cardiac iron load using cardiac MRI T2*. Patients with evidence of any heart failure were excluded from the study. The study population was asked to undergo an echocardiography within 1 month of undergoing cardiac MRI. Complete M-mode, two-dimensional and Doppler echocardiography were performed at rest and by one observer. Data were analyzed as a whole, correlating ultrasound measurements with cardiac R2* by means of regression analysis. In this study, no echocardiographic measurement was seen to efficiently predict an iron-free state. Despite its limitations in screening for early myocardial iron deposition, TDE was however established to be useful in monitoring for progression of iron-induced cardiac dysfunction and response to iron chelation therapy. Patients with decreased LV systolic function may be considered to have iron overload and thus should undergo intense chelation therapy. Once a patient is established to have cardiac siderosis, several echocardiographic criteria may be useful for monitoring [14].
Echocardiography in thalassemic patients on blood transfusions and chelation without heart failure. Rodrigues A, Guiamaraes-Filho F, Braga JC, Rodrigues CS, Waib P, Fabron-Junior A, Tan DM, Franca A, Okoshi M, Okoshi K
This prospective observational study by Rodrigues et al aimed to evaluate cardiac anatomy and function in 18 TM patients who underwent regular blood transfusion and without any evidence heart failure. The study population was matched with two control groups (one with healthy individuals and one with iron deficiency anemia). This was done for the purpose of separately evaluating the effects of anemia and blood transfusion per se. Through different echocardiographic parameters, it was found that conventional Doppler echocardiography and TDI allowed identification of changes in left ventricular diastolic function in asymptomatic TM patients. No significant differences were found in left ventricular structure and systolic function indices [15].
Assessment of methodological quality
QUADAS (quality assessment of diagnostic accuracy studies) criteria
QUADAS scores were tallied in Supplementary 1.
The QUADAS published in 2003 was developed to assess the quality of primary research studies of diagnostic accuracy. The criteria consists of 14 components under three overall criteria: 1) reporting of selection criteria, 2) description of index test execution and 3) description of reference standard execution. Validated scores lie in the range of 0-14 and accordingly, studies are of good quality if at least 7 out 14 criterions are met. In our investigation, the articles appraised were all rated as high quality (Supplementary 1).
| Results | ▴Top |
Evaluation of LVEF (%)
Assumption: Decreased LVEF in thalassemia patients receiving regular transfusions correlates with iron overload as confirmed by CMR T2* < 20 ms.
Our analysis of LVEF in patients with thalassemia showed significant decrease probably due to iron loading when patients with abnormal T2* were compared with patients with normal T2*, at least in Barzin et al and Rodrigues et al’s studies (Fig. 2). Results showed that patients with some degree of iron overload, evident in CMR T2* < 20 ms, had a statistically significant decrease in LVEF with an overall MD of -3.84 (-5.85, -1.83) (Z = 3.75, P = 0.0002). (Good correlation. Relationship: Decreased LVEF among thalassemia patients on regular transfusion may indicate significant iron overload).
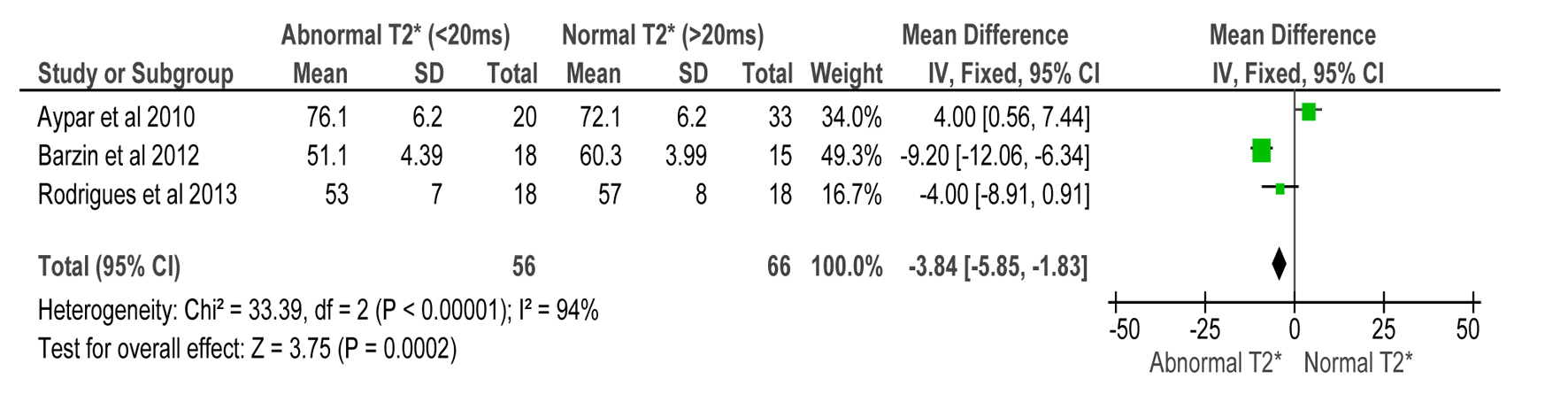 Click for large image | Figure 2. Forest plot of comparison: 1 TDI parameters, outcome: 1.1 LVEF (%) compared to CMR T2* in detecting myocardial iron overload. |
Evaluation of Tei index
Assumption: Increase in Tei index among thalassemia patients on regular transfusion correlates with/indicates iron overloading as confirmed by CMR T2* < 20 ms
Our evaluation of Tei index and its correlation with T2* < 20 ms showed increased values in iron overloaded patients with abnormal T2*. Results suggest that increased Tei index in thalassemia patients may be a TDI marker for increased myocardial iron load (MD 13.03 (9.77, 16.99), Z = 7.83, P < 0.00001) (Fig. 3).
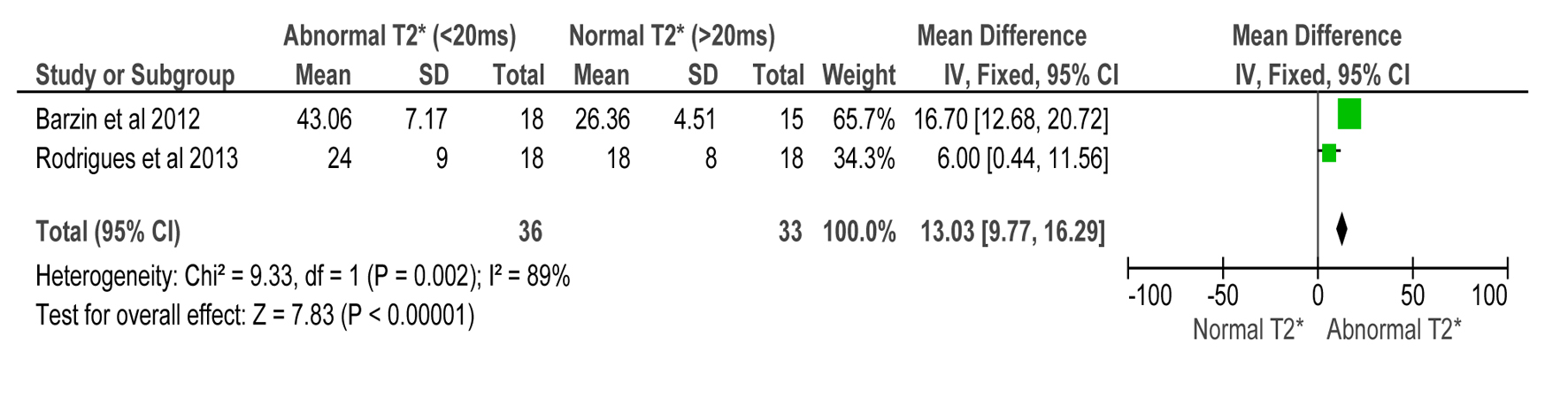 Click for large image | Figure 3. Forest plot of comparison: 1 LVEF (%), outcome: 1.2 Tei index compared to CMR T2* in detecting myocardial iron overload. |
Evaluation of E/A ratio
Assumption: Diastolic dysfunction increases in incidence among iron overloaded thalassemia patients, therefore, E/A ratio is expected to decrease in this subset of patients when compared to normal controls (CMR T2* > 20 ms) as confirmed by T2* < 20 ms.
There was no difference in E/A ratio of normal subjects versus iron overloaded patients (MD 0.18 (0.09, 0.27)) and therefore is not a reliable parameter to gauge myocardial iron overload (Z = 3.88, P = 0.0001) (Fig. 4).
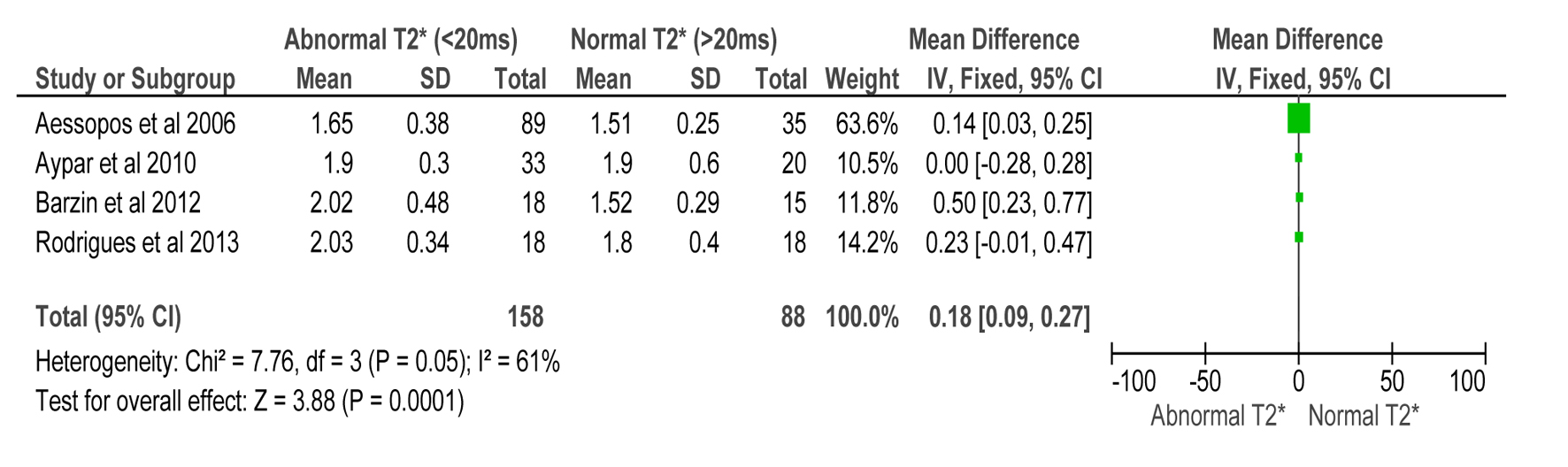 Click for large image | Figure 4. Forest plot of comparison: 1 TDI parameters, outcome: 1.3 E/A ratio compared to CMR T2* in detecting myocardial iron overload. |
Evaluation DT
Assumption: Shortening of DT is indicative of a “restrictive” filling pattern and was found to correlate with iron overload. Therefore, shortened DT among thalassemia patients on regular transfusion may signify iron overload as confirmed by T2* < 20 ms, and may be used as a screening parameter for myocardial iron overload.
DT in abnormally iron loaded patients were shorter in majority of patients in the included studies (MD -27.10 (-33.50, -20.71)). Hence, shorter DT among this subset of patients may be an indicator or myocardial iron overload (Z = 8.31, P < 0.00001) (Fig. 5).
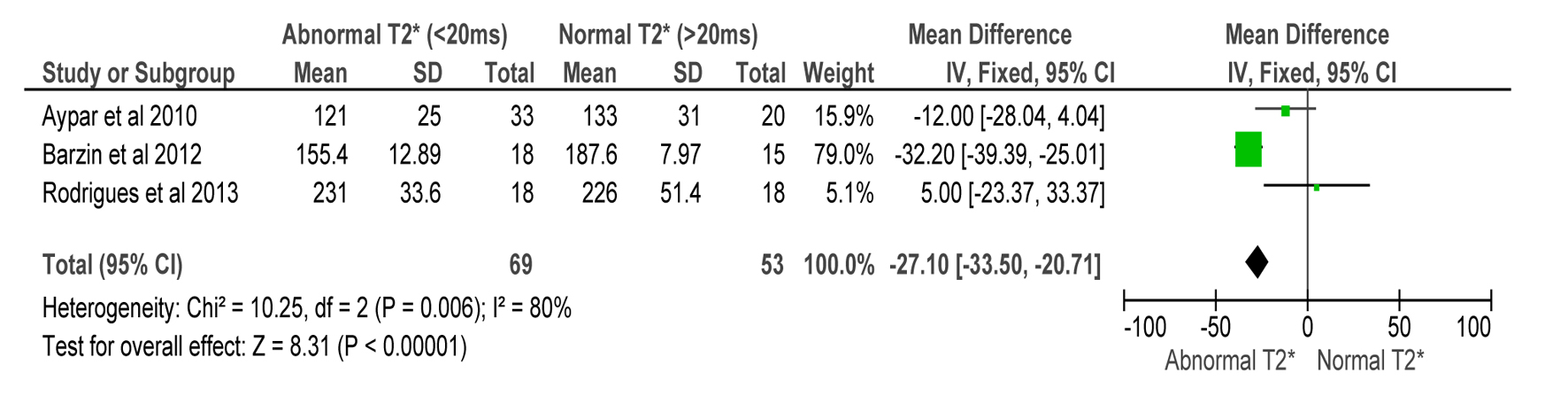 Click for large image | Figure 5. Forest plot of comparison: 1 TDI parameters, outcome: 1.4 deceleration time (ms) compared to CMR T2* in detecting myocardial iron overload. |
Conclusion
In this meta-analysis, several echocardiographic parameters were chosen and analyzed in comparison with cardiac MRI findings to detect myocardial iron overload in thalassemia patients who undergo regular blood transfusion. Tissue Doppler parameters that were seen to have good correlation with the current gold standard are Tei index, DT and LVEF, as summarized in Figure 6. In our present setting, where cardiac MRI is available in only a few institutions and carries a significant burden of cost, these tissue Doppler indices may be used as screening parameters to detect early myocardial iron overload, especially in asymptomatic patients. Significant findings in these studies may likewise be used for monitoring the course of these patients, including their response to iron chelation therapy. These parameters were however only compared to cardiac MRI which is still the gold standard in detection and quantification of myocardial iron loading.
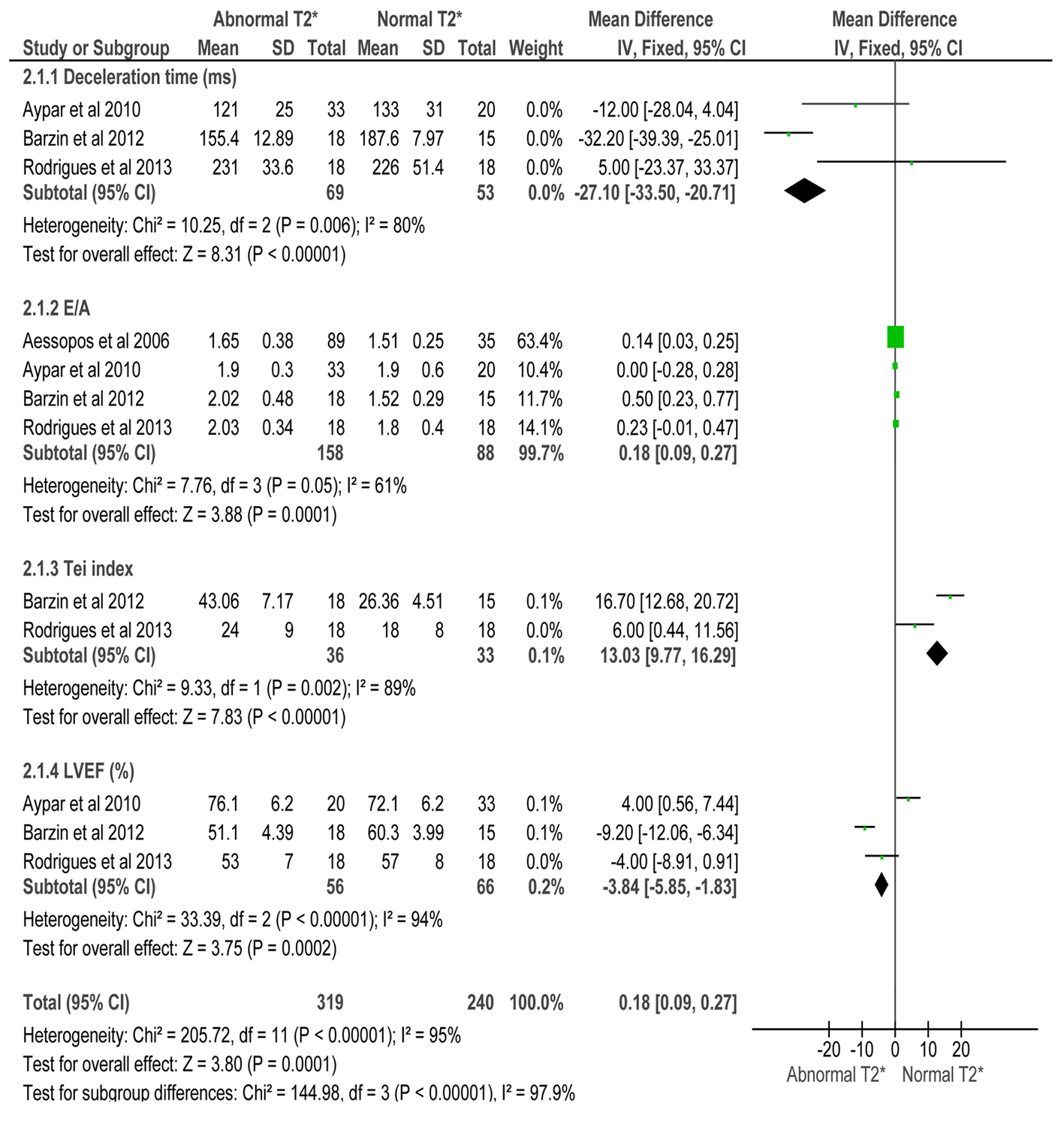 Click for large image | Figure 6. Forest plot of comparison: 2 TDI parameters compared to CMR T2* in iron overloaded thalassemia patients, outcome: 2.1 TDI parameters. |
Recommendations
The meta-analysis only included published free full text articles in English retrieved through online database search and is limited to comparable variables reported in the studies included. In addition, since the articles included did not publish raw data to enable us to determine the overall sensitivity and specificity of tissue Doppler, we were not able to generate a pooled analysis on its accuracy as well as a summary receiver operating characteristic analysis. Alternatively, we used the MD to determine change in the parameters studied (LVEF, Tei index, E/A ratio and DT) to correlate it with myocardial iron overload confirmed on cardiac MRI.
Definition of Terms
1) Tei index - Tei index (TI) also referred to as myocardial performance index, is defined as the sum of isovolumic ventricular contraction time (IVCT) and isovolumic ventricular relaxation time (IVRT) divided by ejection time (ET). It is a Doppler derived unit-less index and is a measure of combined systolic and diastolic myocardial performance of the left ventricle (LV) or right ventricle (RV).
2) E/A ratio - E/A ratio is the ratio of the early (E) to late (A) ventricular filling velocities. The reversal of the E/A ratio (“A” velocity becomes greater than “E” velocity) is often accepted as a clinical marker of diastolic dysfunction, in which the left ventricular wall becomes so stiff as to impair proper filling, which can lead to diastolic heart failure.
3) Deceleration time - The deceleration time (DT) is the time taken from the maximum E point to baseline. Shortening of the DT of the early filling wave is indicative of a “restrictive” filling pattern.
| References | ▴Top |
- Rachmilewitz EA, Giardina PJ. How I treat thalassemia. Blood. 2011;118(13):3479-3488.
doi pubmed - Yuson E. First Pan Asia Conference 2011. Thalassemia Center of the Philippines and Balikatang Thalassemia.
- Ko TM, Caviles AP, Jr., Hwa HL, Liu CW, Hsu PM, Chung YP. Prevalence and molecular characterization of beta-thalassemia in Filipinos. Ann Hematol. 1998;77(6):257-260.
doi pubmed - Borgna-Pignatti C, Rugolotto S, De Stefano P, Piga A, Di Gregorio F, Gamberini MR, Sabato V, et al. Survival and disease complications in thalassemia major. Ann N Y Acad Sci. 1998;850:227-231.
doi pubmed - Li CK, Luk CW, Ling SC, Chik KW, Yuen HL, Shing MM, Chang KO, et al. Morbidity and mortality patterns of thalassaemia major patients in Hong Kong: retrospective study. Hong Kong Med J. 2002;8(4):255-260.
- Spirito P, Lupi G, Melevendi C, Vecchio C. Restrictive diastolic abnormalities identified by Doppler echocardiography in patients with thalassemia major. Circulation. 1990;82(1):88-94.
doi pubmed - Suarez WA, Snyder SA, Berman BB, Brittenham GM, Patel CR. Preclinical cardiac dysfunction in transfusion-dependent children and young adults detected with low-dose dobutamine stress echocardiography. J Am Soc Echocardiogr. 1998;11(10):948-956.
- Kremastinos DT, Tsetsos GA, Tsiapras DP, Karavolias GK, Ladis VA, Kattamis CA. Heart failure in beta thalassemia: a 5-year follow-up study. Am J Med. 2001;111(5):349-354.
doi - Barzin M, Kowsarian M, Akhlaghpoor S, Jalalian R, Taremi M. Correlation of cardiac MRI T2* with echocardiography in thalassemia major. Eur Rev Med Pharmacol Sci. 2012;16(2):254-260.
pubmed - Kondur AK, Li T, Vaitkevicius P, Afonso L. Quantification of myocardial iron overload by cardiovascular magnetic resonance imaging T2* and review of the literature. Clin Cardiol. 2009;32(6):E55-59.
doi pubmed - Olivieri NF, Brittenham GM. Iron-chelating therapy and the treatment of thalassemia. Blood. 1997;89(3):739-761.
pubmed - Aypar E, Alehan D, Hazirolan T, Gumruk F. The efficacy of tissue Doppler imaging in predicting myocardial iron load in patients with beta-thalassemia major: correlation with T2* cardiovascular magnetic resonance. Int J Cardiovasc Imaging. 2010;26(4):413-421.
doi pubmed - Daibiran M, Jalalian R, Karami H, Kowsarian M, Ahmadi A, Shokohi L. Evaluation of diagnostic power of Tissue Doppler Echocardiography for assessment of cardiac iron overload in patients with Thalassemia Major. Int J Hematol Oncol Stem Cell Res. 2012;6:14-19.
- Aessopos A, Giakoumis A, Fragodimitri C, Karabatsos F, Hatziliami A, Yousef J, Gotsis E, et al. Correlation of echocardiography parameters with cardiac magnetic resonance imaging in transfusion-dependent thalassaemia major. Eur J Haematol. 2007;78(1):58-65.
doi pubmed - Rodrigues A, Guimaraes-Filho FV, Braga JC, Rodrigues CS, Waib P, Fabron-Junior A, Tan DM, et al. Echocardiography in thalassemic patients on blood transfusions and chelation without heart failure. Arq Bras Cardiol. 2013;100(1):75-81.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Hematology is published by Elmer Press Inc.